Hysterolaparoscopy Surgery: Procedure, Benefits, and Role in Infertility Diagnosis
Hysterolaparoscopy is a surgery that combines hysteroscopy and laparoscopy to examine the uterus, fallopian tubes, and pelvic cavity. It is often recommended to diagnose and sometimes treat conditions affecting female fertility.
It offers a complete view of the reproductive organs, which helps doctors to identify structural abnormalities, adhesions, or other issues that might impact a woman’s ability to conceive. This article covers various aspects of hysterolaparoscopy, including its purpose, procedure, cost, recovery, and role in infertility treatment.
What is Hysterolaparoscopy?
Hysterolaparoscopy is a diagnostic procedure that combines two techniques: hysteroscopy and laparoscopy.
A hymenoplasty also known as a hymen repair surgery, is a cosmetic procedure which helps to restore the torn hymen. There is no particular reason for a person to get this except for to deal with the social stigma associated with virginity.
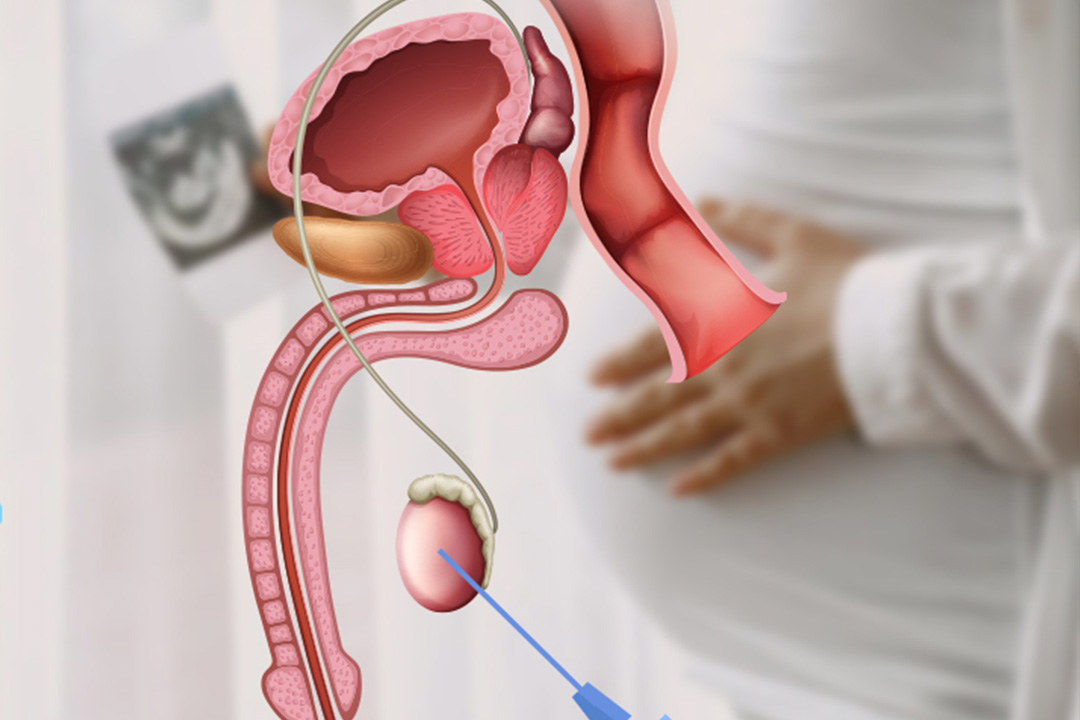
Hysteroscopy involves inserting a small camera through the cervix into the uterus to observe its lining, looking for issues like polyps, fibroids, or abnormal growths.
Laparoscopy uses a tiny camera inserted through a small incision in the abdomen to examine the external structure of the uterus, fallopian tubes, and ovaries. This approach allows doctors to identify pelvic adhesions, endometriosis, or other potential obstructions.
They display close-up images of the inside of the uterus and neighboring reproductive organs, revealing structural issues, scars or adhesions, or inflammation that can impair fertility or cause pelvic pain and heavy periods.
Hysterolaparoscopy in Infertility Diagnosis
Hysterolaparoscopy is commonly performed to evaluate infertility as it finds out some of the potential causes which non-invasive tests like ultrasound or magnetic resonance imaging may fail to pick up. In this regard, it is particularly useful for women with infertility problems or seeking repeated miscarriage. Conditions often identified during hysterolaparoscopy that may impact fertility include:
- Endometriosis: This condition occurs when tissue similar to the uterine lining grows outside the uterus, causing pain and potentially impacting fertility.
- Pelvic Adhesions: Scar tissue resulting from previous surgeries, infections, or endometriosis can bind organs together, disrupting reproductive function.
- Blocked Fallopian Tubes: Blockages prevent the egg from traveling through the fallopian tube, impeding fertilization.
- Fibroids and PolypsThese growths in the uterus can interfere with embryo implantation and lead to pregnancy loss.
In many cases, hysterolaparoscopy is recommended after other methods, such as hormone tests and imaging, have not provided conclusive results.
How is Hysterolaparoscopy Done?
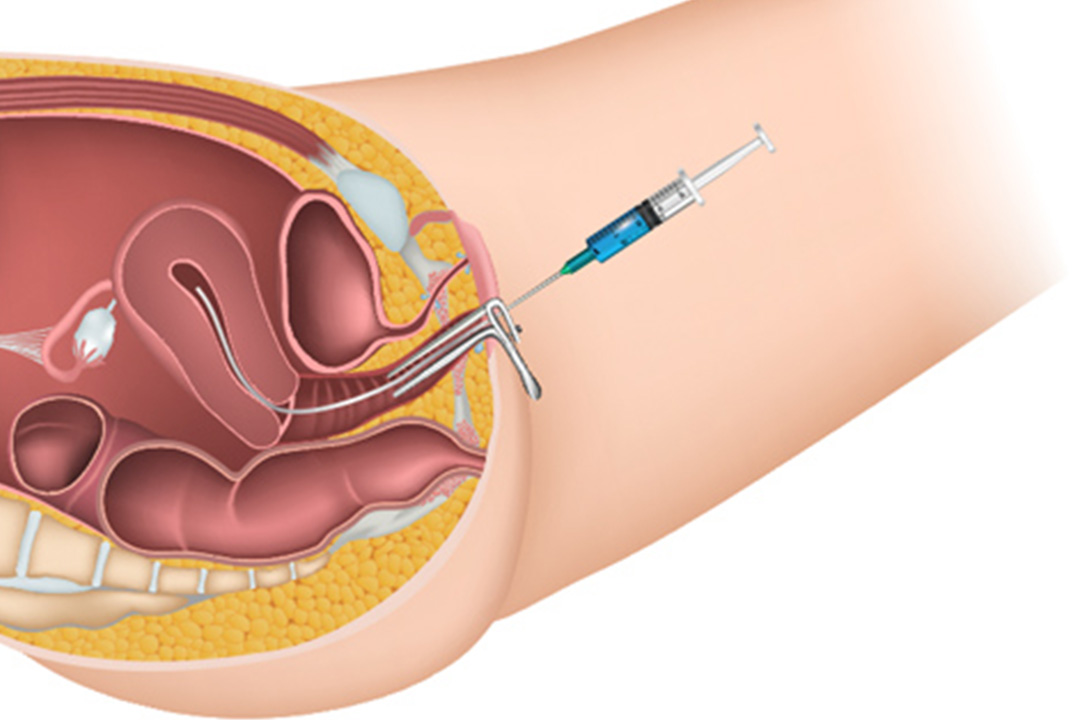
The hysterolaparoscopy procedure is typically performed under general anesthesia to minimize discomfort. Here’s a step-by-step overview:
- Preparation: Before the procedure, the patient is usually asked to fast for several hours, and general anesthesia is administered.
- Hysteroscopy: A small camera known as a hysteroscope is inserted through the cervix into the uterus. It allows the physician to inspect the uterine cavity. The doctor may use a saline solution to expand the uterus for better visibility.
- Laparoscopy: A small incision is made near the navel, and a laparoscope (a thin tube with a camera) is inserted into the abdomen. To improve visibility, carbon dioxide gas is introduced, slightly inflating the abdominal cavity and creating space between the organs.
- Examination and Treatment: The doctor examines the uterus, fallopian tubes, ovaries, and pelvic cavity. If any abnormalities, such as fibroids or adhesions, are found, minor corrective surgery can sometimes be performed during the same session.
- Completion: The laparoscopy and hysteroscopy are removed, and the small abdominal incision is closed with sutures.
The entire procedure takes about 30-45 minutes, and since it is minimally invasive, recovery time is relatively short.
Is Hysterolaparoscopy Painful?
Hysterolaparoscopy is performed under generalized anesthesia, so pain is not expected during the procedure itself.
Mild discomfort or cramps in the pelvic area are expected afterward, whereas some might experience shoulder pain-a result of having used carbon dioxide gas to expand the abdomen-but this usually resolves itself in one to two days.
The use of over-the-counter pain relievers usually helps alleviate such symptoms; therefore, most women can bounce back to their normal life after a few days.
Recovery Time for Hysterolaparoscopy
Recovery from hysterolaparoscopy is generally quick, with most patients able to return home on the same day. However, complete recovery may take a week, depending on the individual and any additional procedures performed. After surgery, patients are advised to:
- Rest and avoid strenuous activities for at least 48 hours.
- Avoid heavy lifting and intense exercise for a week or until advised by their physician.
- Refrain from sexual intercourse for about two weeks to allow the reproductive organs to heal.
It is normal to experience some mild bleeding or spotting for a few days post-procedure. Any severe pain, fever, or heavy bleeding should be promptly reported to a healthcare provider.
Hysterolaparoscopy Cost
Hysterolaparoscopy cost varies based on location, hospital charges, and whether the procedure is pure diagnostic or entails therapy. Generally, the ranges of procedure cost vary from INR 30,000 to INR 70,000. This usually covers anesthesia, surgeon's fees, and the hospital stay if needed.
Hysterolaparoscopy insurance coverage will depend on health insurance policies and whether the procedure will be covered as medically necessary in regard to infertility diagnosis or treatment. It is recommended that prior communication with the healthcare provider and insurance company be made to ascertain coverage and avoid bills that are higher than expected.
The Role of Hysterolaparoscopy in Pregnancy
Hysterolaparoscopy is one of the most important fertility-enhancing procedures as it enables doctors to both diagnose and treat conditions that may impede pregnancy.
Hysterolaparoscopy can help enhance a woman's conception chances by correcting such problems as endometriosis, adhesions, or fibroids. Several studies suggest that for many women, fertility increases once conditions discovered during hysterolaparoscopy are treated.
Hysterolaparoscopy does not guarantee pregnancy, but it provides very useful information concerning the reproductive organs and is often done with a view toward achieving pregnancy.
A few women perform this test as part of the pre-IVF evaluation process, whereby doctors assure that uterine and fallopian tube conditions are optimal before other treatment options such as IVF are started.
What Makes Hysterolaparoscopy Different from Other Diagnostic Methods?
Hysterolaparoscopy has this unique advantage over other non-invasive imaging techniques like ultrasound or MRI: it allows direct visual inspection of the reproductive organs in real-time.
It also allows diagnosis and treatment in one step, depending on the need, which means it is efficient in saving women such as those suffering from infertility and other unexplained reproductive health issues.
For instance, if a possible fibroid was detected by ultrasound, only hysterolaparoscopy can confirm this finding and then immediately remove the offending lesion. This approach will expedite diagnosis and therapy and avoid any additional surgical procedures.
Hysterolaparoscopy for Surgery and Treatment
Hysteroscopy is primarily done to aid diagnosis, but can also serve as a therapeutic device. Where the clinician finds such conditions as polyps, fibroids, adhesions, or endometriosis, they can often deal with those during the same procedure.
Adhesions can be cut away, polyps or fibroids removed, and other findings that may impair fertility treated with the aid of small instruments. It helps combine the surgical approach of an exploratory laparotomy, minimally invasive procedure for diagnosis and treatment, hence lessening the need for a second surgery.
Hysterolaparoscopy Method: Minimally Invasive and Effective
The minimally invasive nature of hysterolaparoscopy makes it a preferred option for diagnosing infertility-related conditions. The small incisions reduce scarring, recovery time, and postoperative complications, making it a relatively safe choice with a quick turnaround for patients.
Conclusion
Hysterolaparoscopy is a potent instrument of diagnosis and treatment and an invaluable tool in infertility diagnosis and treatment disorders concerning reproductive health. This procedure is well tolerated, minimally invasive, and often provides an immediate diagnosis and treatment.
Though the thought of surgery may be daunting, the procedure itself is quite safe, effective, and almost painless as anesthesia combined with the use of small incisions. Recovery is usually very rapid with most women able to return to normal within about a week.
It can prove to be a solution for women suffering from infertility or unexplained fertility conditions and thus enable them to know better about their body.
They might end up increasing their chances of getting pregnant, and women looking forward to building a family may consult a knowledgeable reproductive health expert to decide whether the technique is something appropriate for them.
References

About Us
AKsigen IVF is a premier center for advanced fertility treatments, with renowned fertility experts on our team. Specializing in IVF, ICSI, egg freezing, and other cutting-edge reproductive technologies, AKsigen IVF is committed to helping couples achieve their dream of parenthood. With personalized care and a patient-first approach, AKsigen IVF provides comprehensive fertility solutions under one roof.