What is the Next Step after Follicular Study?
The follicular study is an important stage to determine a woman's fertility. It monitors the growth of ovarian follicles that contain mature eggs. This ultrasound-based evaluation helps to identify the best time for ovulation. It also helps fertility doctors to prescribe the right medications.
However, understanding the next steps following a follicular study is important for couples hoping to conceive. The journey does not end with the follicular study.
This article discusses the next stages after a follicular study, with a focus on three popular fertility treatments: intrauterine insemination (IUI), in vitro fertilization (IVF), and intracytoplasmic sperm injection (ICSI). Couples can increase their chances of having a successful pregnancy by looking into these options.

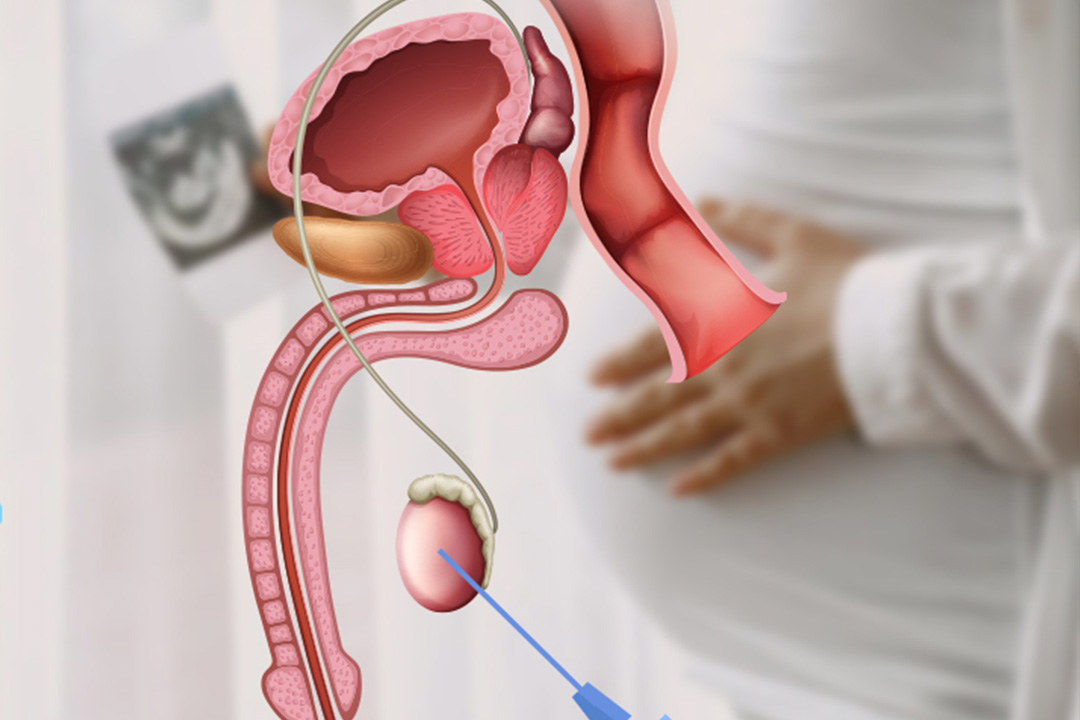
IUI – Intrauterine Insemination
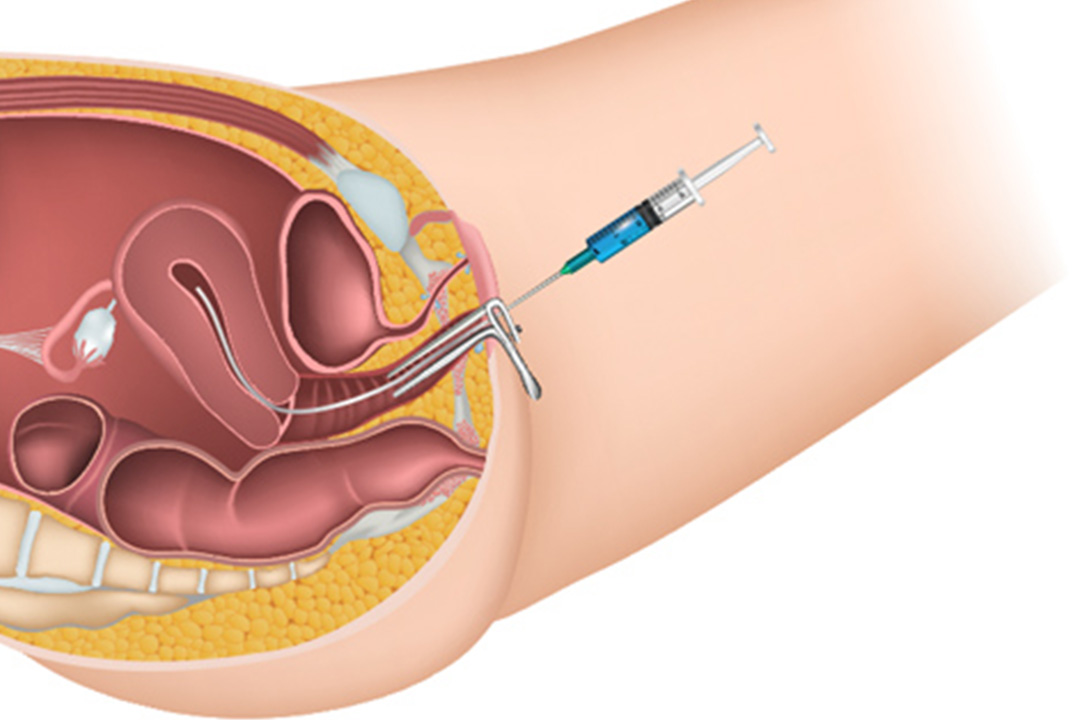
Intrauterine insemination (IUI) is usually the first treatment advised after a follicular study. Particularly when natural conception chances are poor or impossible to achieve. IUI is more suited for couples with a female partner under 40 years old. This method includes using fertility medicines to stimulate the ovaries. It is followed by observing follicular studies to determine the exact timing of ovulation.
Semen is first extracted from the male partner. It then undergoes a 'washed' cycle to separate higher-quality sperm from lower-quality sperm. This provides a much higher possibility of successful fertilization. Meanwhile, the female partner's ovulation cycle is examined and timed for the best insemination time. When follicles are prepared, a catheter is introduced via a thin procedure to implant the washed sperm directly inside the uterus.
The application of IUI is advised based on a few conditions such as:
- mild male factor infertility
- cervical factor infertility
- ovulatory disorders
- semen allergies
- requirement of using donor sperm
- infertility problems related to endometriosis
IUI is a least invasive procedure. IUI does not require any type of hospitalization. IUI is less costly, simple in its nature, and therefore one of the appealing procedures for a lot of those facing infertility.
In-Vitro Fertilization
IVF is used when IUI is not possible or ineffective. A follicular study is carried out first. IVF is the process of fertilizing a woman's eggs with sperm outside her body in a controlled laboratory setting. It is more costly and intrusive than IUI but has higher success rates. It is particularly for couples with more serious fertility problems.
IVF begins with ovarian stimulation with fertility medications, which leads to the development of multiple eggs. Follicular studies guarantee that mature eggs are collected around ovulation. A small surgical technique called egg retrieval is used to extract eggs from the ovaries.
Fertilization occurs when eggs and sperm are combined in a laboratory dish. After fertilization, developing embryos are cultured.
After successful fertilization, one or more viable embryos are chosen and implanted in the woman's uterus. It is done by using a simple, non-invasive technique. If implantation happens, a pregnancy occurs. IVF is especially advised for women:
- over the age of 40
- blocked or damaged fallopian tubes
- genetic diseases
- severe endometriosis
- decreased sperm production or function in the male partner
Additionally, IVF is often chosen by couples who have already tried and failed other fertility treatments.
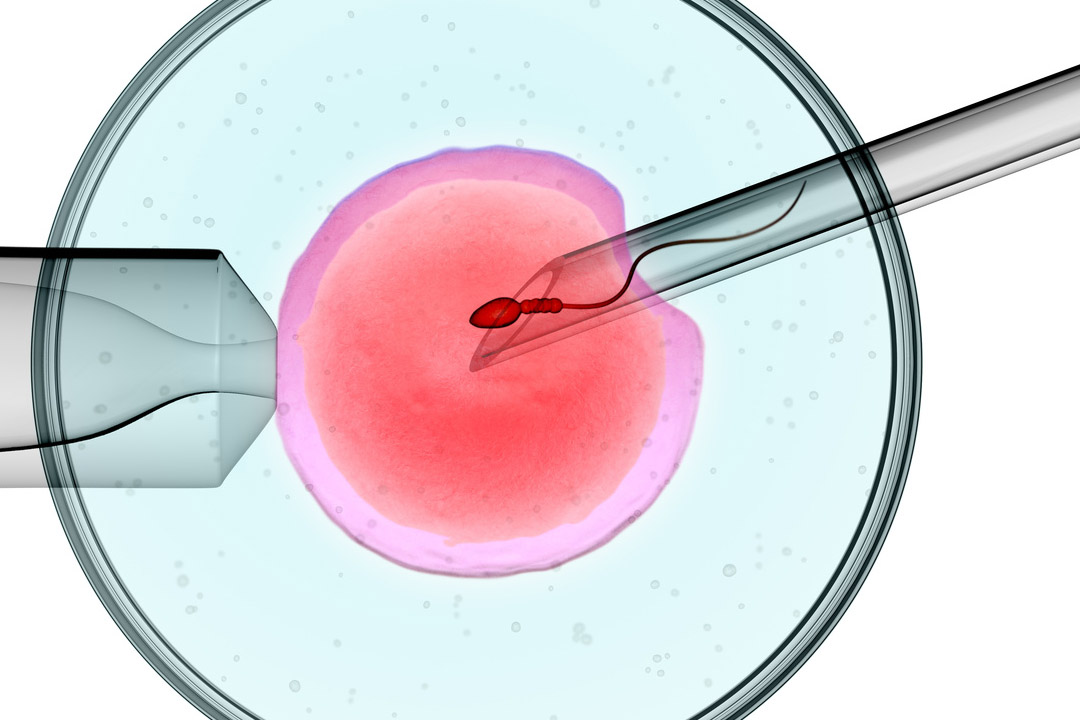
ICSI – Intracytoplasmic Sperm Injection
This is a technique of IVF that is a specialized procedure often recommended in a situation where there may be a very significant male-factor infertility.
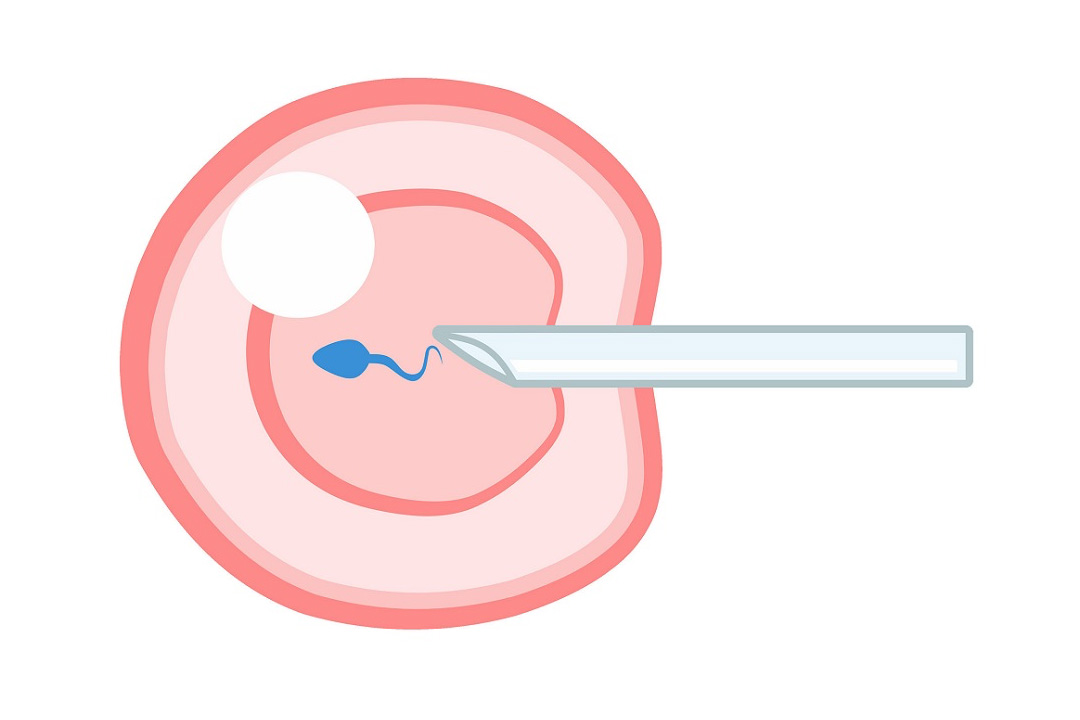
Here, ICSI directly injects a single sperm inside an egg allowing fertilization. This increases the rate of fertilization especially in serious male factor conditions.
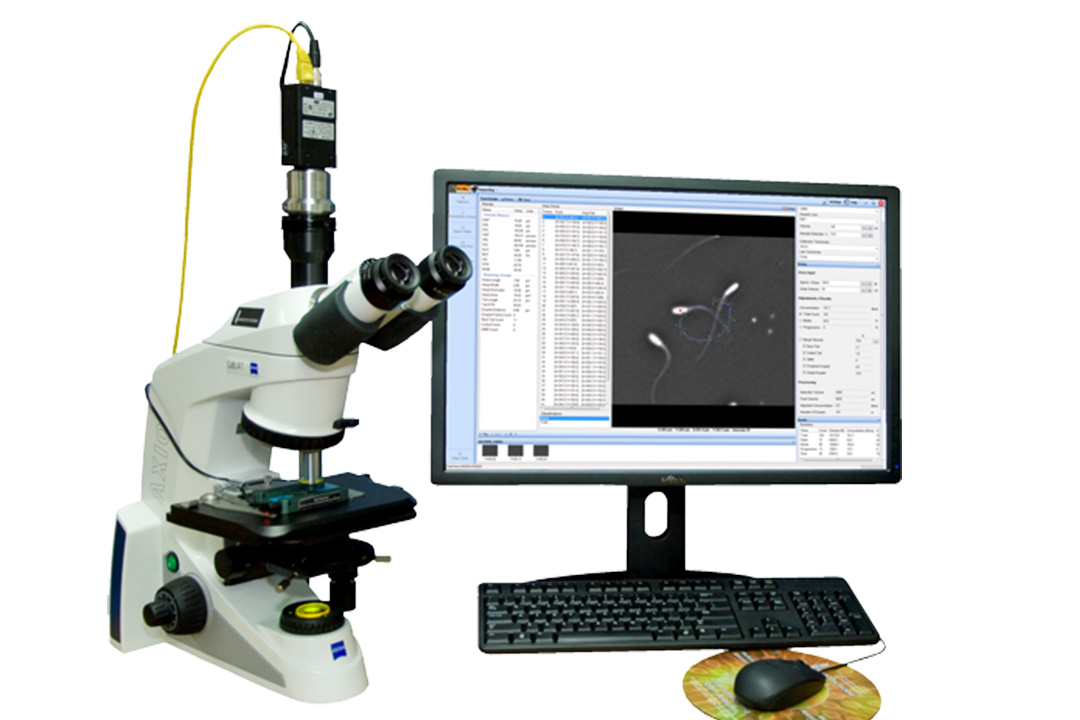
The ICSI treatment is initiated similar to IVF. Stimulation of the ovaries and retrieval of mature eggs is done first. But instead of allowing sperm to fertilize eggs naturally in a dish, a single sperm is injected under a microscope through a fine needle into each egg.
This helps bypass barriers, such as low sperm count, poor sperm motility, or abnormal sperm morphology, ensuring even sperm with the least fertility potential can achieve fertilization.
ICSI is recommended in several conditions such as:
- very low sperm counts
- poor motility
- abnormal shape
- previous failed attempts of IVF
- genetic abnormalities affecting the sperm
It can also be used in situations where surgical sperm retrieval is required due to blockages or absence. ICSI is also beneficial in frozen sperm applications.
It guarantees that conserved genetic material can still be used for fertilization. The breakthrough technology has changed fertility treatments, giving hope to many couples with severe male infertility.
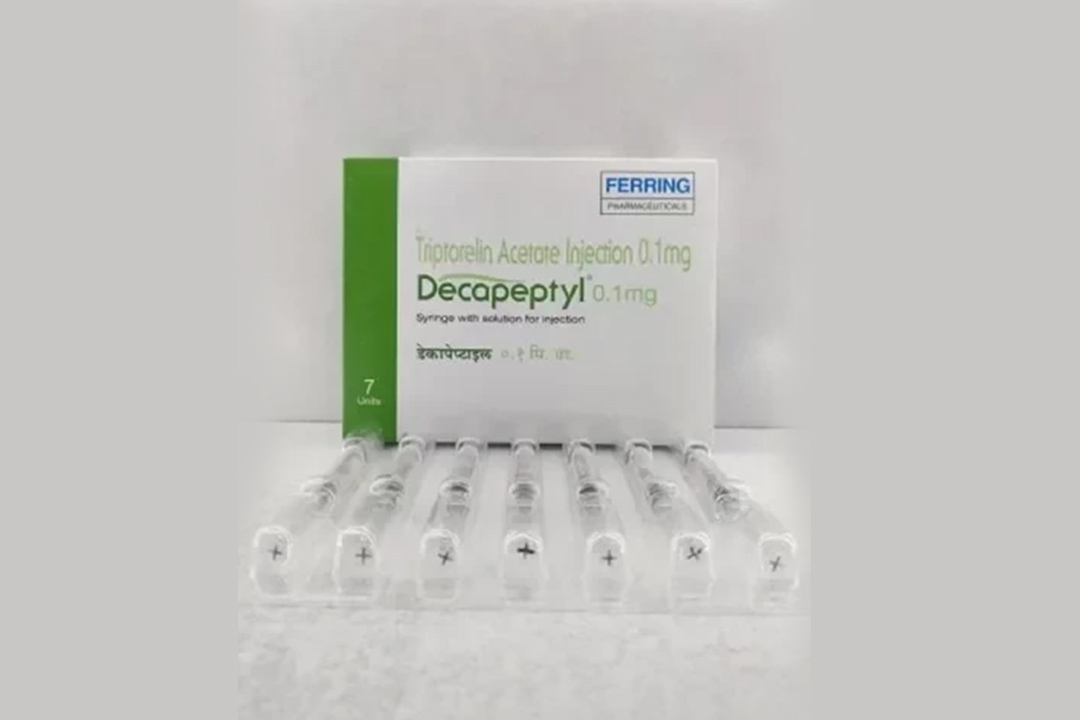
HCG Injection after Follicular Study
HCG injections play an important role in fertility treatment procedures following a follicular study. HCG causes the final maturation of the eggs.
Thus, causes ovulation to be induced to get them ready for insemination or retrieval. The time for giving HCG injections has to be precise so that it will fall exactly in sync with the time when the follicles are prepared.
HCG is injected when the follicles are at the desired size while monitoring follicular growth with ultrasonography and hormone levels. This injection replaces the naturally occurring LH surge that triggers ovulation.
It ensures that eggs are mature at the time of retrieval in IVF or natural release in timed intercourse and IUI treatments. Proper HCG delivery is required to match ovulation with the fertility treatment. This increases the likelihood of successful fertilization and implantation.
Other Considerations After a Follicular Study
Besides IUI, IVF, and ICSI, several other factors and treatments may be considered after a follicular study to enhance fertility outcomes. These include:
Healthy lifestyle habits, such as a balanced diet, regular exercise,no smoking and excessive alcohol consumption can improve fertility. Weight management is also important because both underweight and overweight conditions can affect ovulation and hormonal balance.
In case of structural defects such as a blocked fallopian tube or fibroids in the uterus, the only option left is surgery to correct the abnormalities. Once the normal anatomy of the reproductive organs is re-established chances of fertility greatly improve.
Genetic Testing
Genetic testing is recommended to couples who have a history of genetic disorders or recurrent miscarriages. Identifying and addressing genetic issues can prevent the transmission of hereditary conditions and improve the chances of a healthy pregnancy.
Fertility treatments can be emotionally challenging. Seeking psychological support through counseling or support groups can help couples cope with the stress and emotional toll of infertility treatments.
Success Rates and Considerations
The success rates of fertility treatments after a follicular study vary with factors such as age, underlying fertility issues, and the specific treatment used. IUI generally has a success rate of 10-20% per cycle. It makes it a suitable first-line treatment for many couples.
IVF provides for better success, often ranging 30-40% per cycle, and more commonly utilized where couples face several challenges toward conception. ICSI, as the special version of IVF, further enhances such cases with males facing major complications, increasing its success rate above IVF on its own.
Several cycles may be necessary to gain a successful pregnancy; the cost can become overwhelming in a short time. These procedures may take significant physical and emotional tolls. There is a place for couples to share these considerations with their fertility specialists so that informed decisions are made that fit each couple's specific situation and circumstances.
Preparing for Fertility Treatments
Preparation is essential in maximizing the success of fertility treatments following a follicular study. Couples must be prepared to face this process, both physically and emotionally. The following are some steps that can be considered:
- Both couples must have a full medical assessment to identify whether they have any issues that may affect fertility. To increase your chance of success, these conditions should be addressed before starting fertility therapy.
- These therapies involve major expenses that can be addressed by suitable financial plans. They involve having proper insurance coverage or other programs that will cover your multiple attempts.
- Knowledge of the different kinds of fertility treatments, procedures, success rates, and possible risks may allow couples to make wise choices.
Conclusion
It is a difficult effort to go on through the process of conception. Once a couple understands what steps are required after the follicular study, their chances of a successful pregnancy rise greatly.
Intrauterine Insemination (IUI), In Vitro Fertilization (IVF), and Intracytoplasmic Sperm Injection (ICSI) are three of the various fertility therapies, with each providing a specialized treatment for each type of infertility issue. Supportive treatments such as HCG injections, lifestyle changes, and psychological assistance are all necessary for fertility therapy.
Interaction between the couple and fertility experts on the different options helps them in making the right choice based on their specific situation. Regardless of how tough this procedure appears, the advancement of reproductive technologies provides hope for many people starting families.
About Us
AKsigen IVF is a premier center for advanced fertility treatments, with renowned fertility experts on our team. Specializing in IVF, ICSI, egg freezing, and other cutting-edge reproductive technologies, AKsigen IVF is committed to helping couples achieve their dream of parenthood. With personalized care and a patient-first approach, AKsigen IVF provides comprehensive fertility solutions under one roof.