Trigger Shot in IVF: Everything you need to know
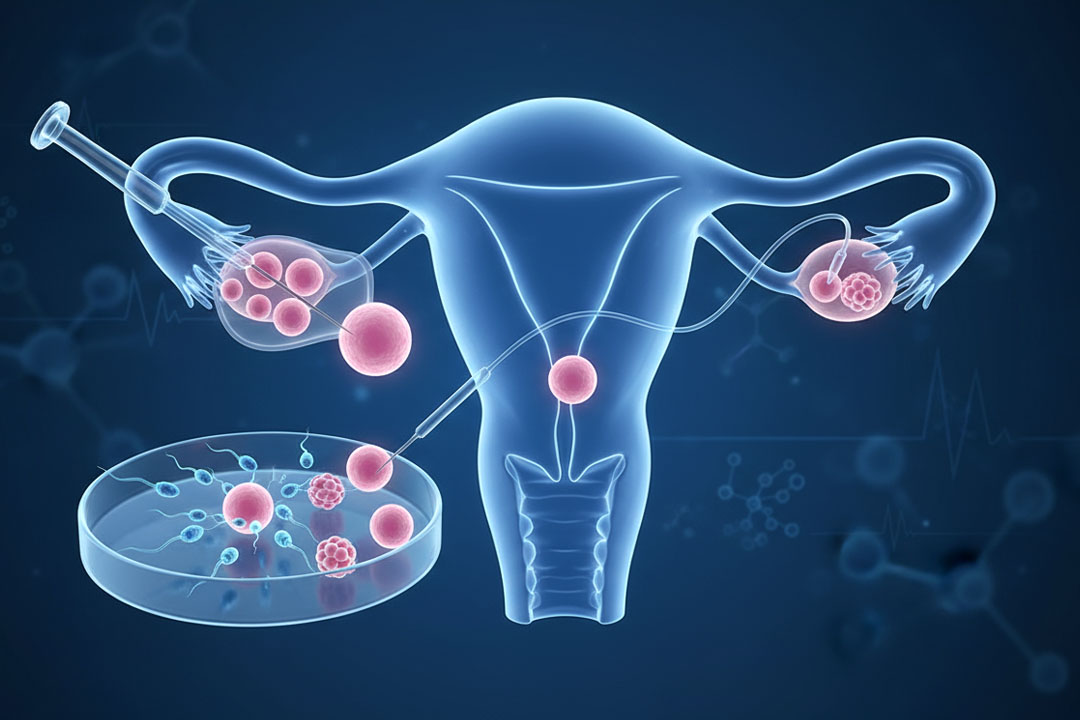
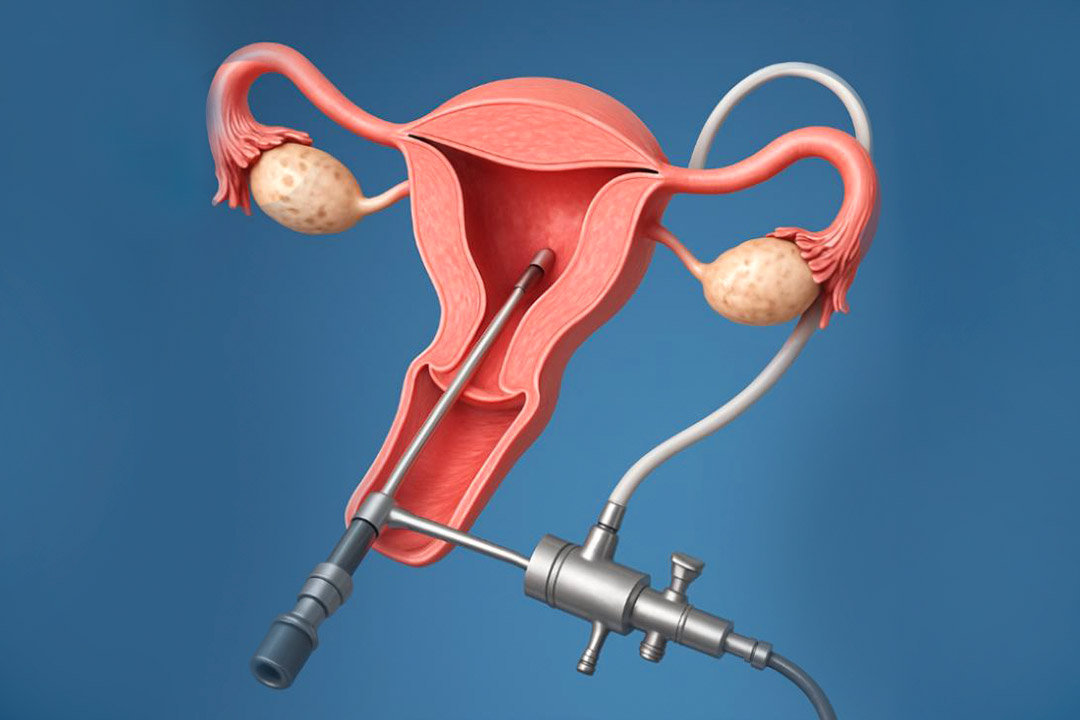
IVF is a procedure that often requires multiple hormonal injections to increase the chances of pregnancy. Among the components of many IVF cycles, it is essential to have 'trigger injection,' as it mimics the body's natural surge of hormones that prepares the body for releasing an egg at the right time for retrieval. Understanding the trigger shot in terms of its mechanism, timing, and possible side effects is considered very important for those undergoing fertility treatments.
The trigger injection can be also administered in timed intercourse and IUI procedures. Through a controlled environment for egg maturation and release, the trigger shot maximizes the chances of proper fertilization and implantation.
In this article, we will explore the function of the trigger injection within IVF, examine how it is administered and timed. Additionally, we will review potential side effects and what patients can expect during this stage of their treatment.
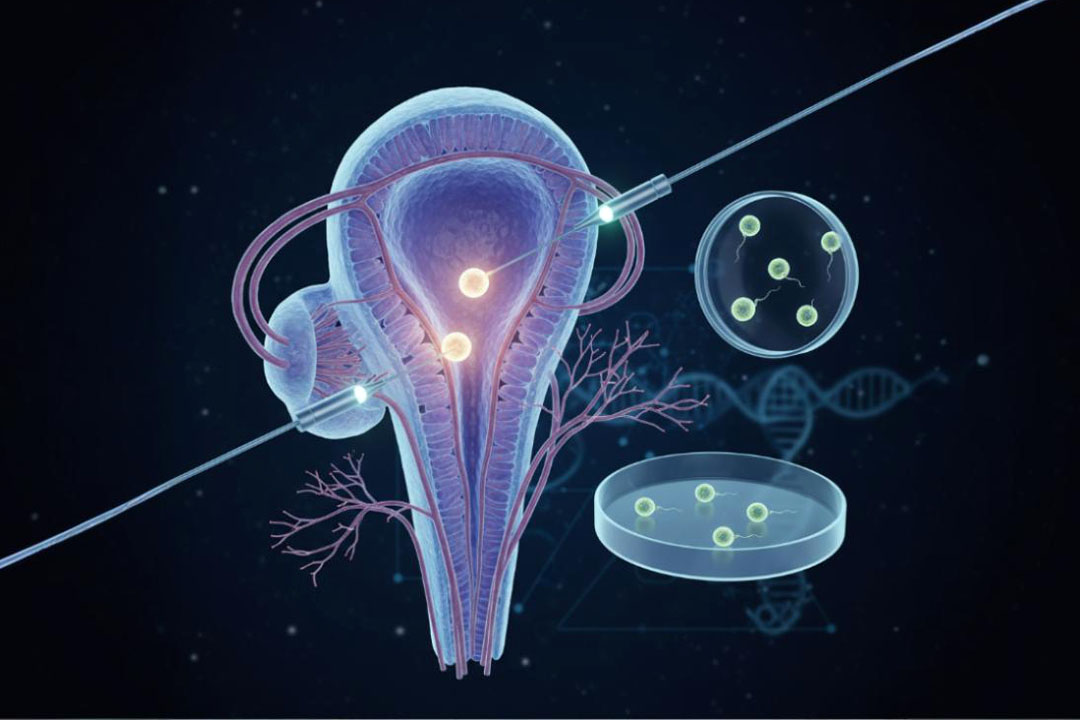
What is a Trigger Injection?
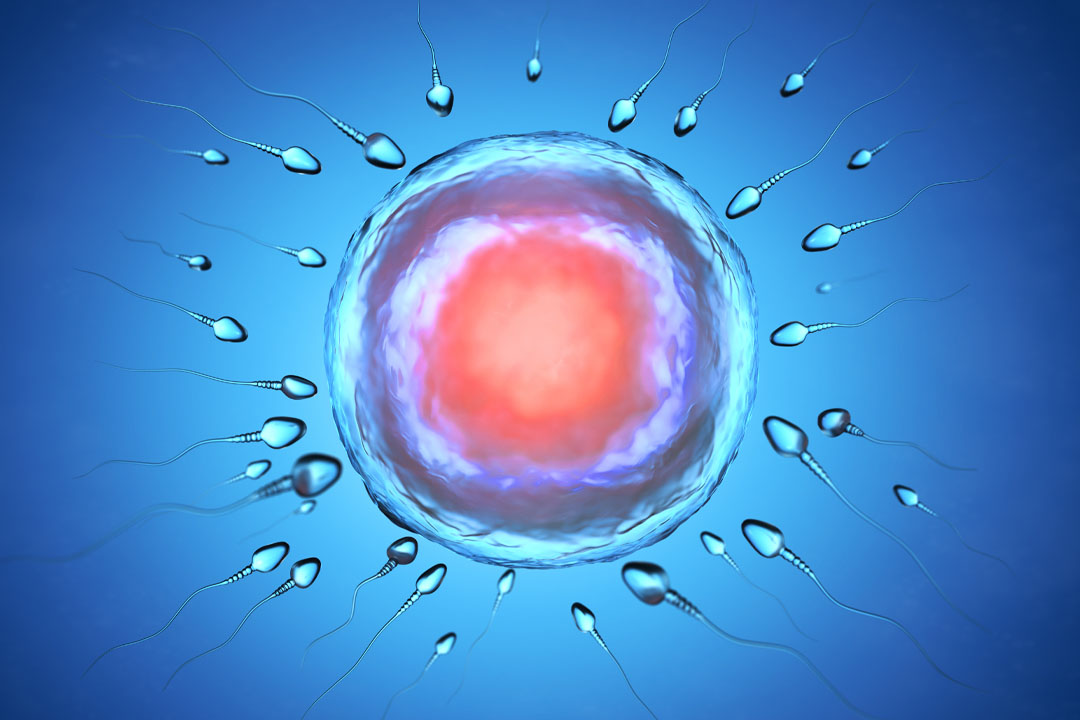
The trigger injection is known by brand names such as Ovidrel, Novarel, or Pregnyl. It contains the hormone human chorionic gonadotropin (hCG). hCG is known as the 'pregnancy hormone,' but in this situation it is applied to mimic LH.
Luteinizing Hormone (LH) a natural hormone secreted by the pituitary gland that triggers the final steps of an egg's maturation and release from an ovary. Administering hCG as a trigger shot can help fertility specialists mimic the LH surge, which matures and then causes the eggs to ovulate in a controlled and predictable manner.
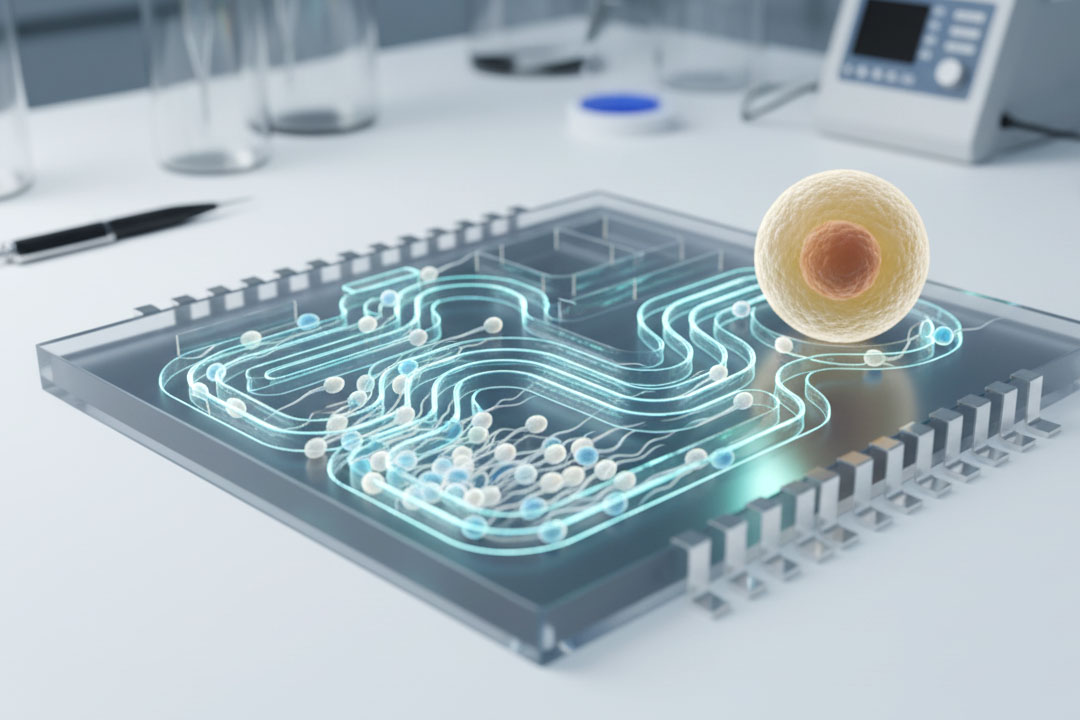
This is one of the methods in a larger class of treatments called gonadotropin therapy, which has been developed over several decades. Gonadotropins stimulate the ovaries to produce mature follicles, and the trigger injection is extremely useful when natural ovulation is either absent or insufficient. The injection also allows for precise timing, which is particularly useful for coordinating procedures such as IUI or egg retrieval for IVF.
Mechanism of Action in IVF
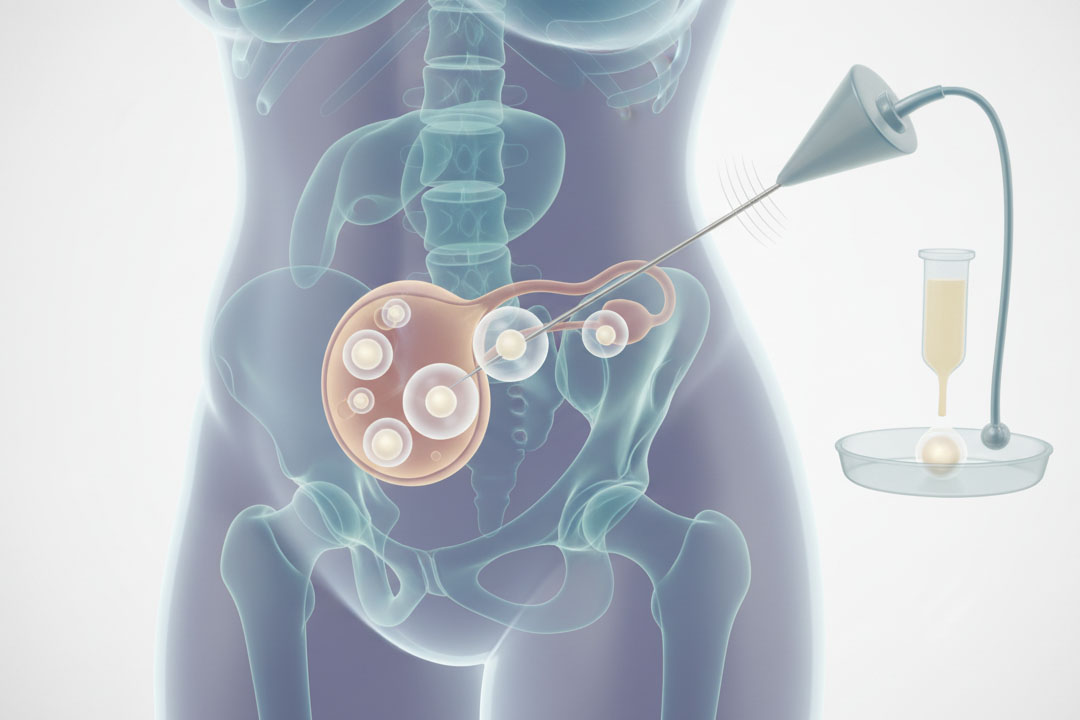
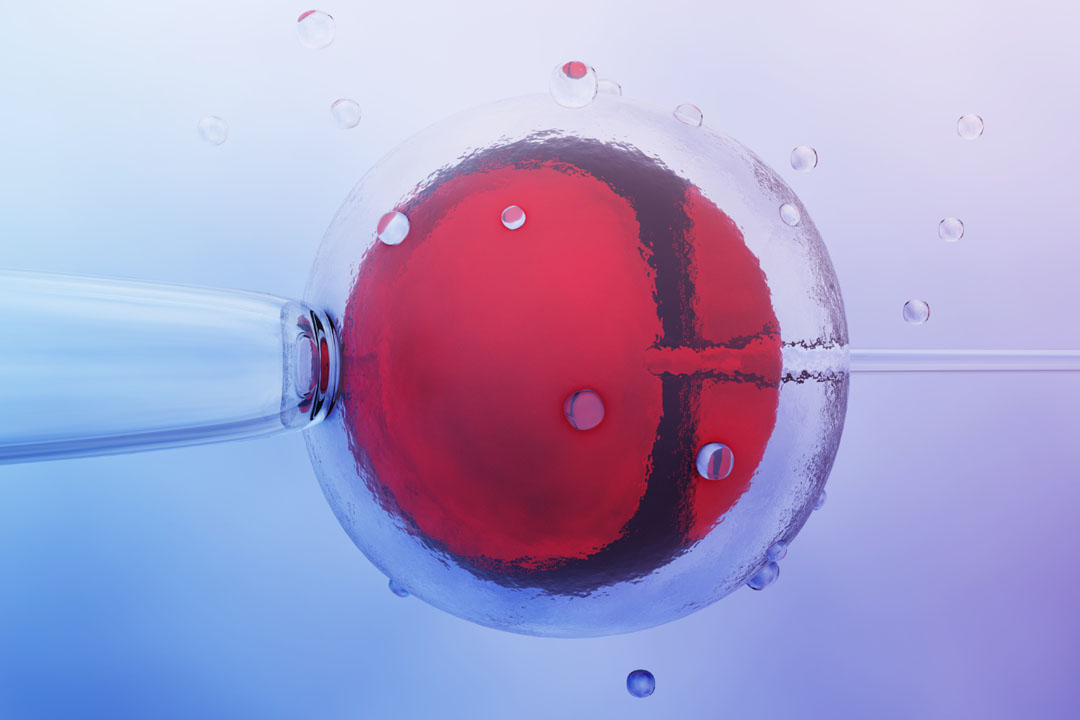
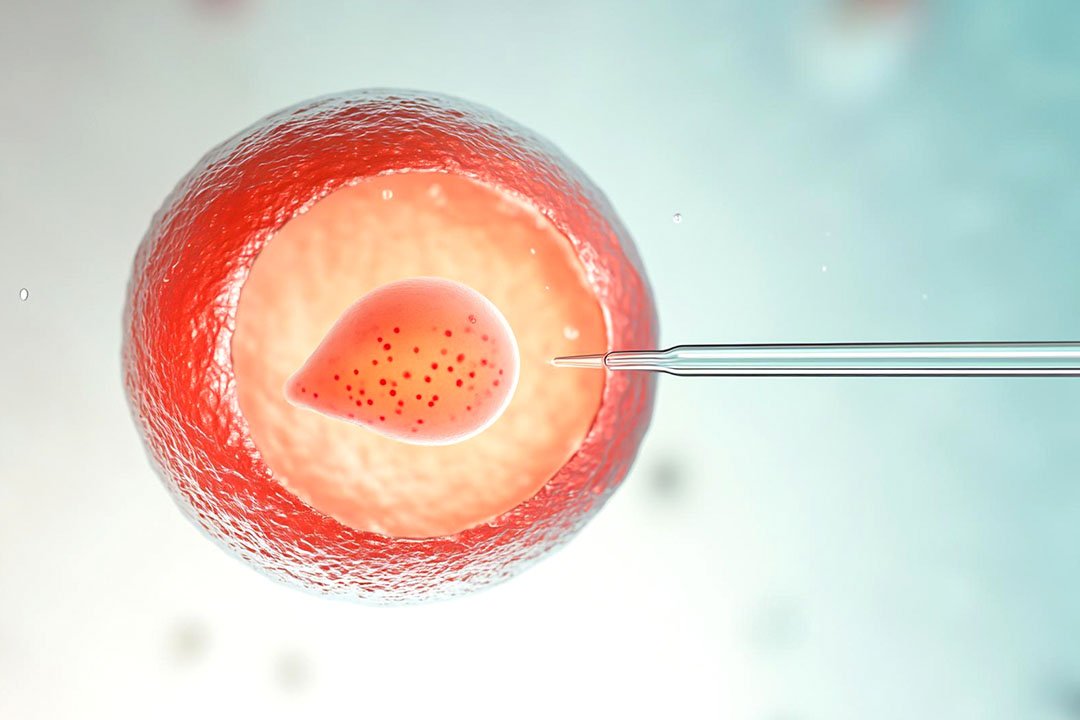
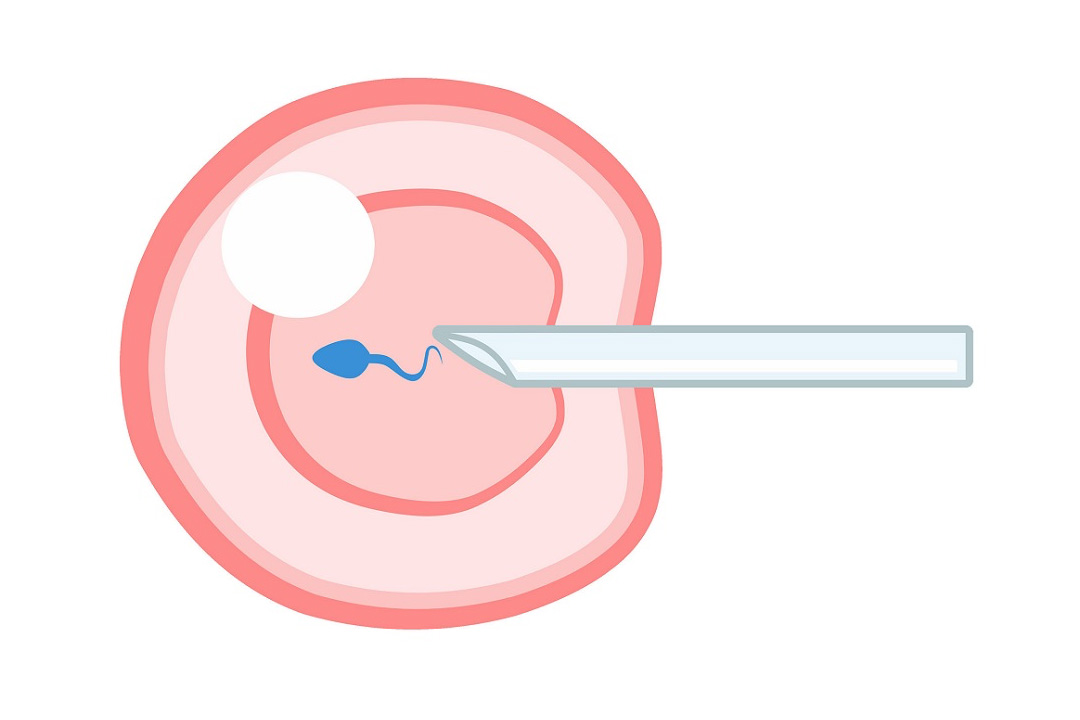
Timing in IVF is important in the procedure to achieve the best results. After ovarian stimulation with medications such as follicle-stimulating hormone (FSH), a trigger shot of hCG is administered when follicles have reached an optimal size. The injection triggers the final stages of egg maturation.
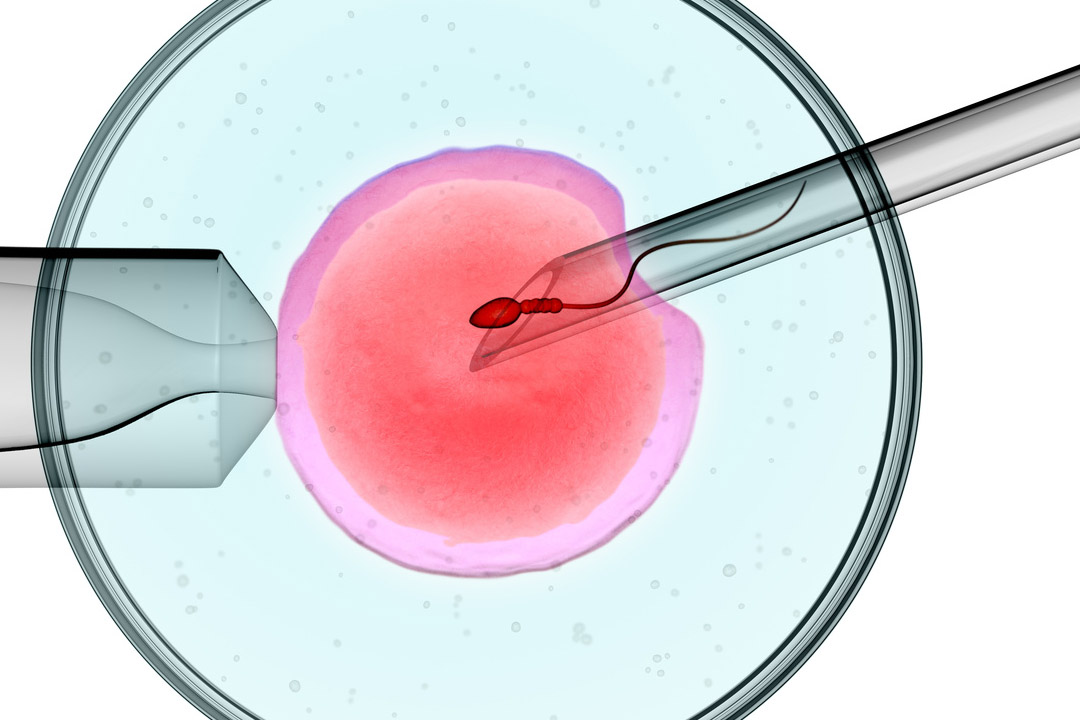
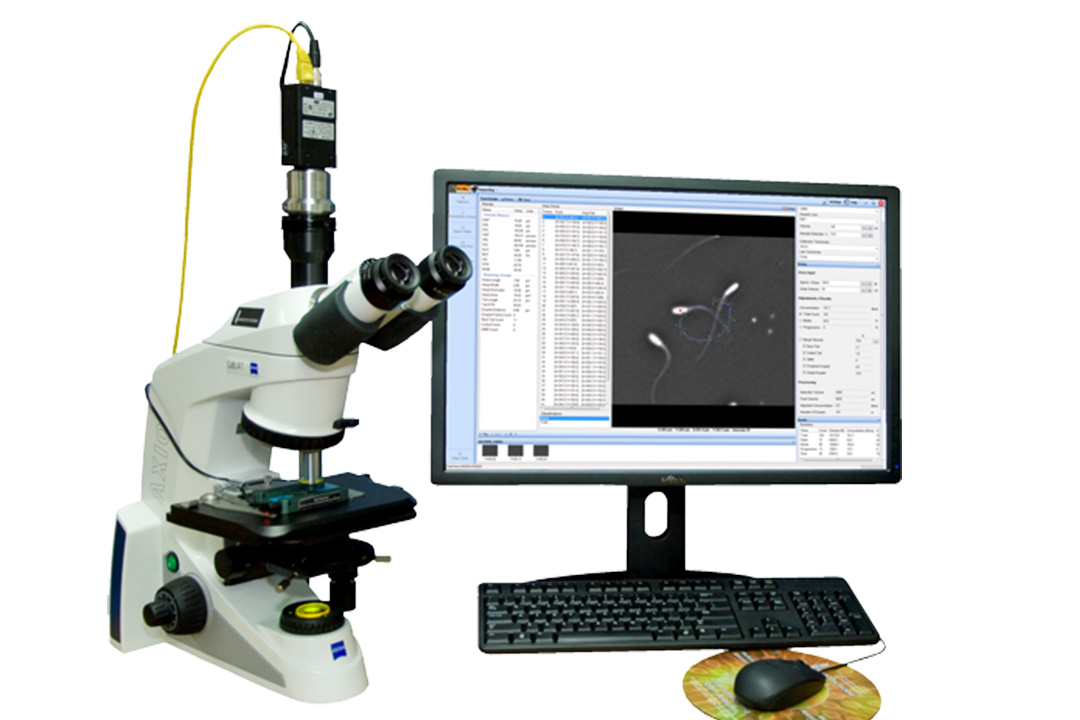
After injection of the trigger, the eggs will mature and will be ready for retrieval. The fertility specialists schedule the collection of eggs around 36 hours after the injection when the eggs will have started to be spontaneously released. This timing is accurate to ensure that the eggs are at the best state possible when they are retrieved and then introduced to the sperm in the laboratory.
Administration and Timing
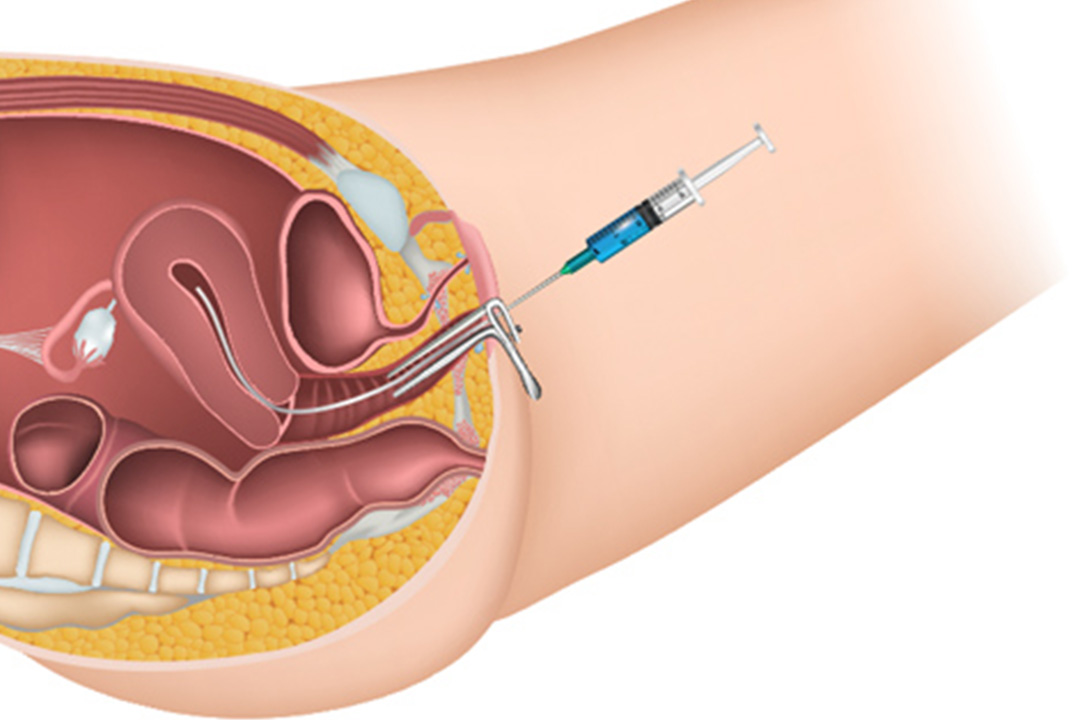
The trigger shot can be administered either intramuscularly or subcutaneously. Many patients prefer the subcutaneous route due to its ease and lower discomfort. Doctors usually educate patients on how to self-administer the shot especially given the importance of timing.
In a standard IVF cycle, the trigger injection is given when the ovarian follicles are of a certain size, usually between 15mm and 22mm. This size is an indication that the eggs inside those follicles are almost mature. The scheduling and careful monitoring of follicle development involve regular ultrasounds and consultations with fertility specialists.
Side Effects and Considerations
Most women experience minimal discomfort during or after the trigger shot. Some common side effects include:
- minor bloating
- slight pain at the injection site
- pelvic discomfort
These sensations are typically temporary and manageable. However, one potential risk associated with trigger injections, particularly when combined with other fertility medications, is ovarian hyperstimulation syndrome (OHSS).
OHSS can range from mild to severe, with symptoms including severe abdominal bloating, pain, nausea, vomiting. In rare cases, serious complications such as blood clots or difficulty breathing.
Patients should monitor their symptoms closely and report any concerning signs to their doctor. Side effects and treatment protocols may need to be altered in such cases if communication with the medical team is not regular.
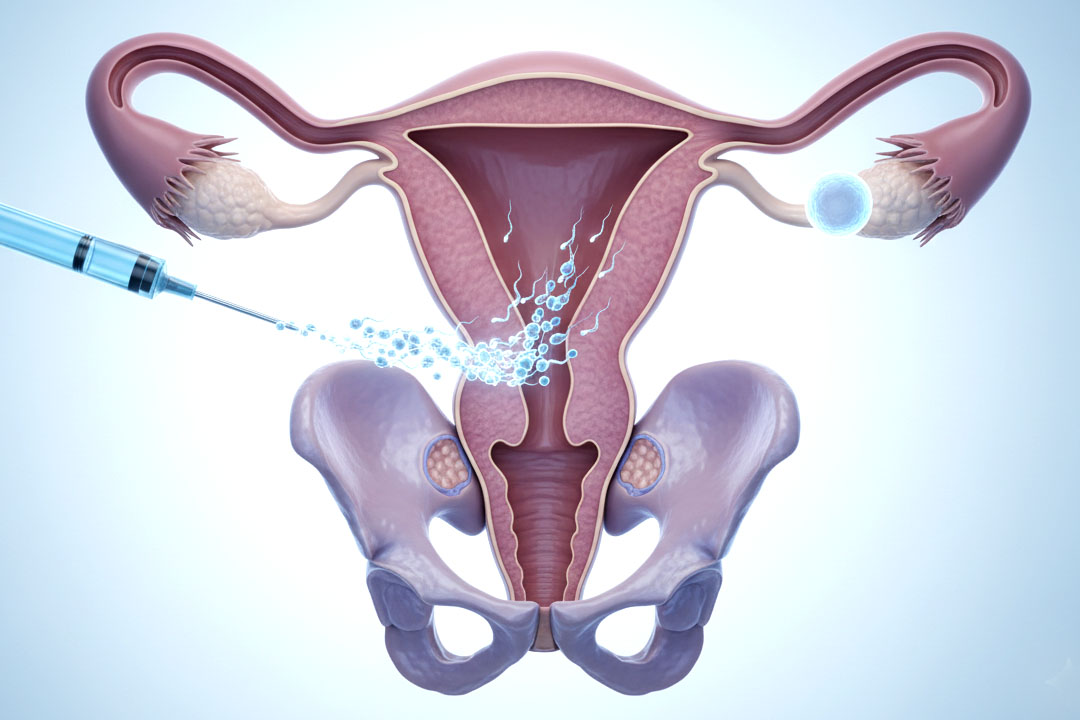
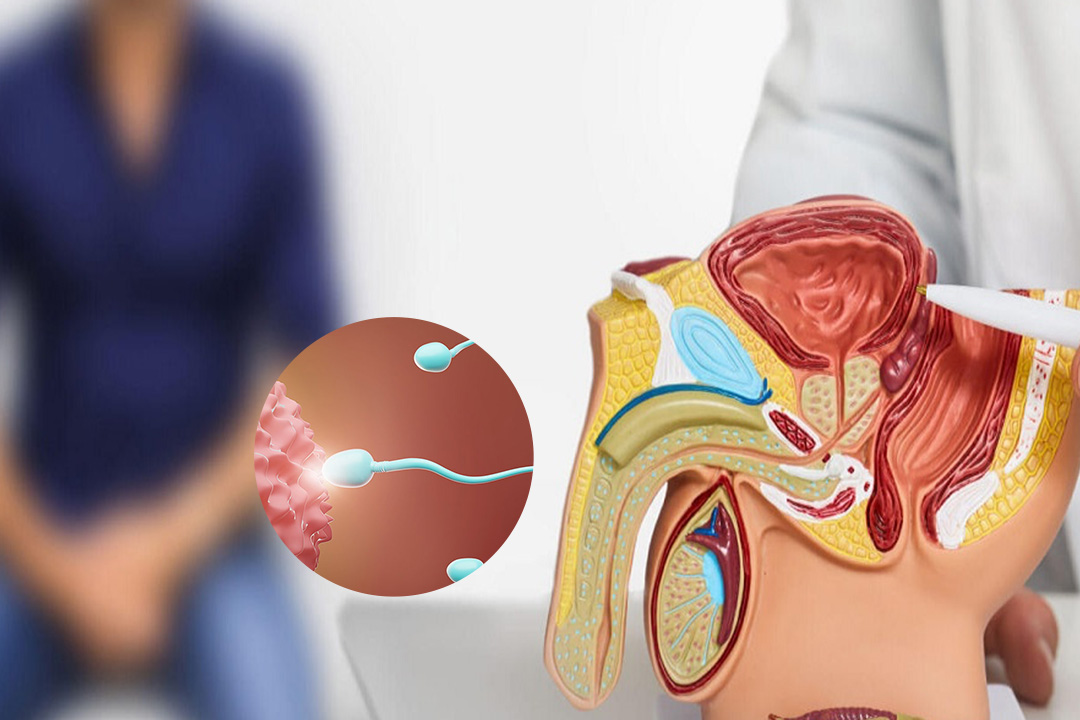
The Role of the Trigger Shot in IUI
The trigger shot is not just used with IVF. It is also administered with timed intercourse and intrauterine insemination (IUI). In these contexts, the injection is used to help time ovulation with planned sexual activity or the timing of an IUI procedure.
When follicles have reached the desired size and the uterine lining is appropriately thick, a professional will instruct the patient to administer the trigger shot. The scheduling of intercourse or IUI usually occurs 24 to 36 hours after the injection. It aligns with the predicted time of ovulation.
In a scientific study, researchers found that application of the trigger shot had dramatically improved success rates during IUI treatments. It works in the context of an expert's accurate prediction of the ovulation period such that the sperms will reach the reproductive tract when there is an excellent opportunity for their fertilizing functions.
Follow-Up and Pregnancy Testing
It is crucial for patients that received a triggering shot to understand how to test for pregnancy and when. Injection will lead to the presence of hCG in the body, giving false positives if one takes the test too early.
Doctors usually advise two weeks after injection before one takes a pregnancy test to confirm that the hormone has worn off from the body. If tests are taken earlier, the results may not accurately reflect a true pregnancy.
Some patients will watch the declining hCG levels and test themselves every day past their expected period. A fading line may indicate that the hormone from the injection is being excreted from the body, whereas a steady or deepening line might be indicative of pregnancy. For certain results, a blood test given by a doctor is the most accurate test.
Impact of the Trigger Shot on Follicular Development
In the context of IVF, the trigger shot also influences the growth of follicles. After administration, follicles can continue to grow for several hours as they approach full maturity. The injection accelerates the process and allows smaller follicles to catch up and reach a size that is optimal for egg retrieval.
This coordination is important because poorly developed or too-mature eggs may decrease the chances of successful fertilization. Through triggering the simultaneous readiness of a group of eggs to that ideal stage, the trigger shot maximizes the egg retrieval process efficiency and increases the possibility of viable embryos for transfer.
Administration Techniques and Pain Management
The technique employed in the injection can impact the pain a patient will endure. Subcutaneous injections are generally less painful and have fewer side effects at the injection site compared to intramuscular injections. Patients often report a mild stinging sensation similar to receiving a routine vaccination.
Addressing Missed Injections
Missing a scheduled trigger shot can be a significant setback in an IVF cycle. If a patient realizes they have missed the optimal time for administering the injection, it is important that they contact their doctor right away. The doctor may be able to adjust the egg retrieval schedule or give alternative instructions to minimize the delay's impact.
The chances of saving the cycle are higher if actions are taken immediately, but there is no guarantee of success. The medical team will assess the situation and advise the best course of action depending on individual circumstances.
Conclusion
The trigger injection is a pivotal step in the IVF process. It plays a central role in preparing eggs for successful retrieval and fertilization. By mimicking the natural LH surge with an hCG injection, the trigger shot ensures that eggs mature properly and are retrieved at the optimal time.
The overall process is not very complicated or dangerous, yet involves careful timing and procedures with perfect communication between a patient and fertility team. Mechanism, time, side effects, and best practice with the trigger injection are all to be understood as a way for patients to self-assure regarding their fertility treatments.
About Us
AKsigen IVF is a premier center for advanced fertility treatments, with renowned fertility experts on our team. Specializing in IVF, ICSI, egg freezing, and other cutting-edge reproductive technologies, AKsigen IVF is committed to helping couples achieve their dream of parenthood. With personalized care and a patient-first approach, AKsigen IVF provides comprehensive fertility solutions under one roof.