Exploring the Different Kinds of IVF
Embryo Transfer in IVF
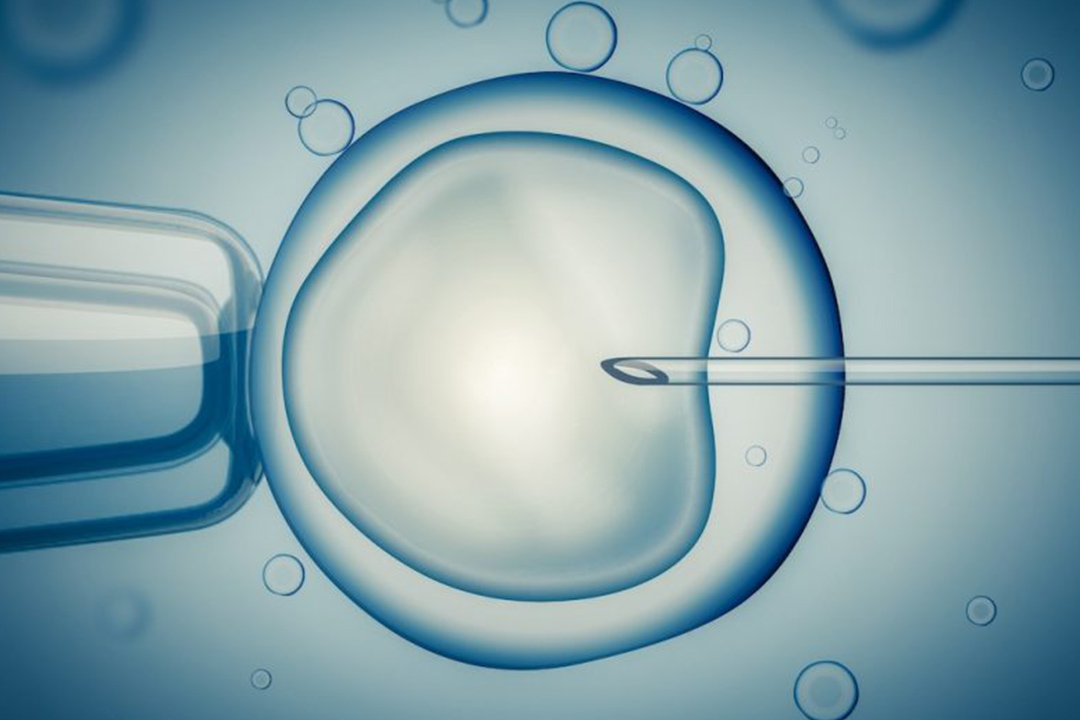
In vitro fertilization is a term that has become very common in modern society. Although the procedure is often referred to as the 'test-tube baby' procedure, it does not involve fertilization or embryo development in an actual test tube. Instead, the term 'in vitro' means 'in glass,' referring to the laboratory dish where fertilization and early embryo growth occur.
Unlike artificial insemination, where the sperms are placed directly inside the uterus, IVF involves mixing eggs and sperms in a controlled laboratory environment. One or more embryos are transferred into the uterus after fertilization and early embryo development to achieve a successful pregnancy.
Even though IVF is a complicated and expensive procedure, it has become an essential choice for approximately 5% of couples suffering from infertility and offers them hope of parenthood when other treatments have failed.
Whether you are considering conventional methods or alternative protocols, understanding these different approaches can help guide you towards the best treatment for your unique circumstances.
Conventional IVF
The most commonly known and practiced form of in vitro fertilization is conventional IVF. In this approach, fertility medications are given to stimulate the ovaries to develop multiple egg follicles.
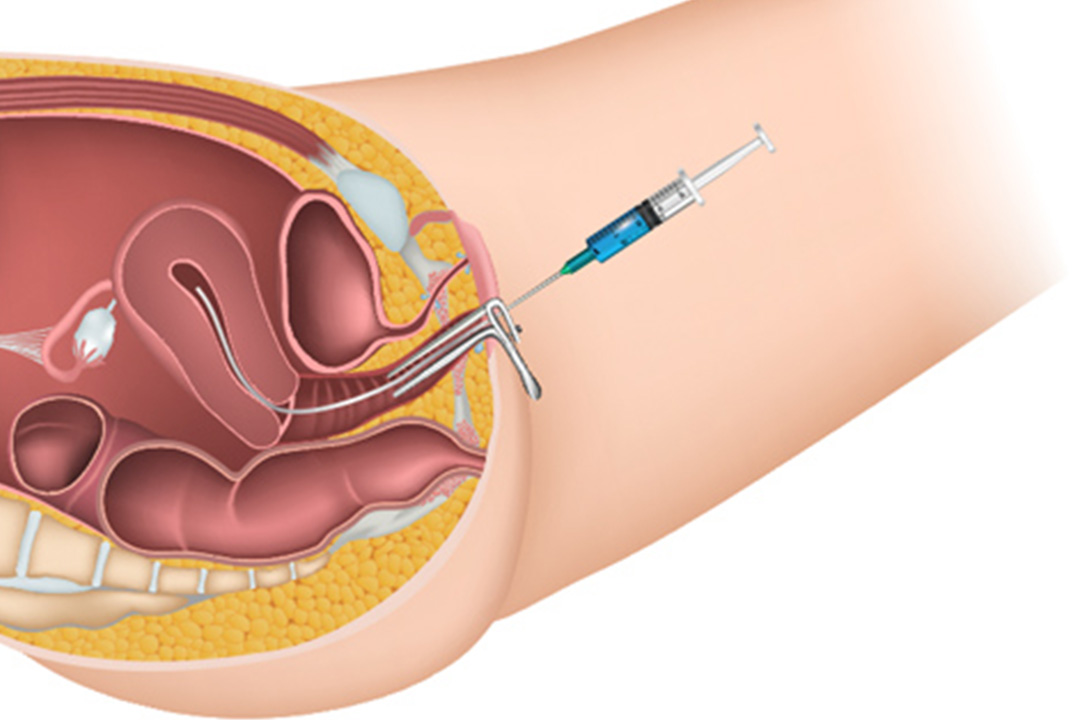
When the eggs are mature, they are retrieved through a minor surgical procedure and fertilized with sperm in a laboratory dish. The resulting embryos are then monitored, and one or more are transferred to the uterus.
This technique is often advised for women with a number of infertility issues, including blockages or damage to the Fallopian tubes, unexplained infertility, or advanced maternal age (typically above 35 years). Couples who have not had success with less invasive techniques like intrauterine insemination may also benefit from traditional IVF.
Although offering a moderate success rate of about 12% per cycle, it remains the standard of care for most because it has established protocols and is well known among specialists.
Natural Cycle IVF
Natural cycle IVF is a more gentle version of traditional IVF that only follows the woman's natural menstrual cycle. Here, stimulating drugs or injections are not used; instead, the whole procedure centers on the observation of one naturally selected egg each month. When the egg is matured to an optimal stage, it is retrieved and is exposed to a sperm in a laboratory before the embryo is transferred into the uterus.
This procedure is most suitable for women who are still in their ovulating phase and would prefer not to take fertility medications, which cause some side effects. It is also preferred in cases where a woman has low ovarian reserve or did not respond well to the high-stimulation protocols.
The body naturally selects what is good for it; hence, natural cycle IVF needs constant observation and is conducted by experienced fertility doctors. The technique is subtle but hopeful, especially for those patients who prefer a more natural treatment regimen.
Minimal stimulation IVF
Minimal stimulation IVF, which is also known as Mini-IVF, or micro-IVF, is similar to conventional IVF except that the dosage of the fertility medications is lower.
This therapy is used to stimulate the ovaries enough to yield a few excellent eggs rather than doing excessive stimulation that can lead to production of a large number of eggs. There is less chance of developing OHSS from this type of therapy, and overall lower treatment costs are usually experienced.
This is often most helpful for women with diminished ovarian reserve or for those who have had problems in the past or poor responses to traditional high stimulation protocols.
Mini-IVF uses fewer medications making the experience less aggressive but focusing on quality rather than quantity. The procedure is good for the woman who wants a more natural, less invasive approach to fertility treatment.
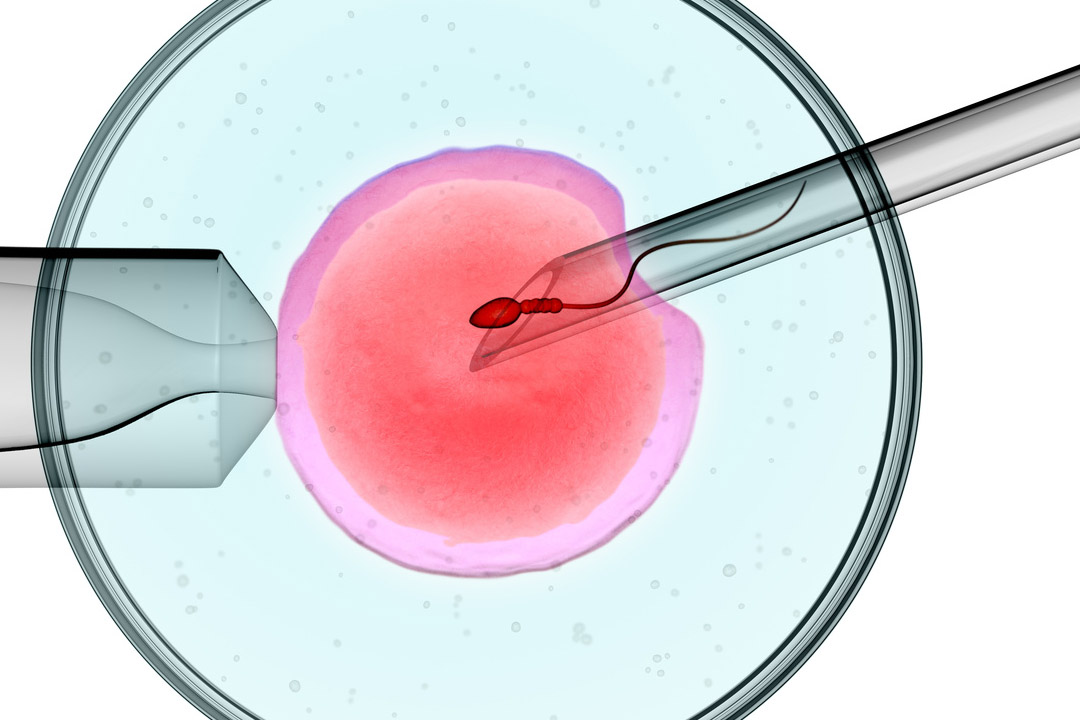
Intracytoplasmic Sperm Injection (ICSI)
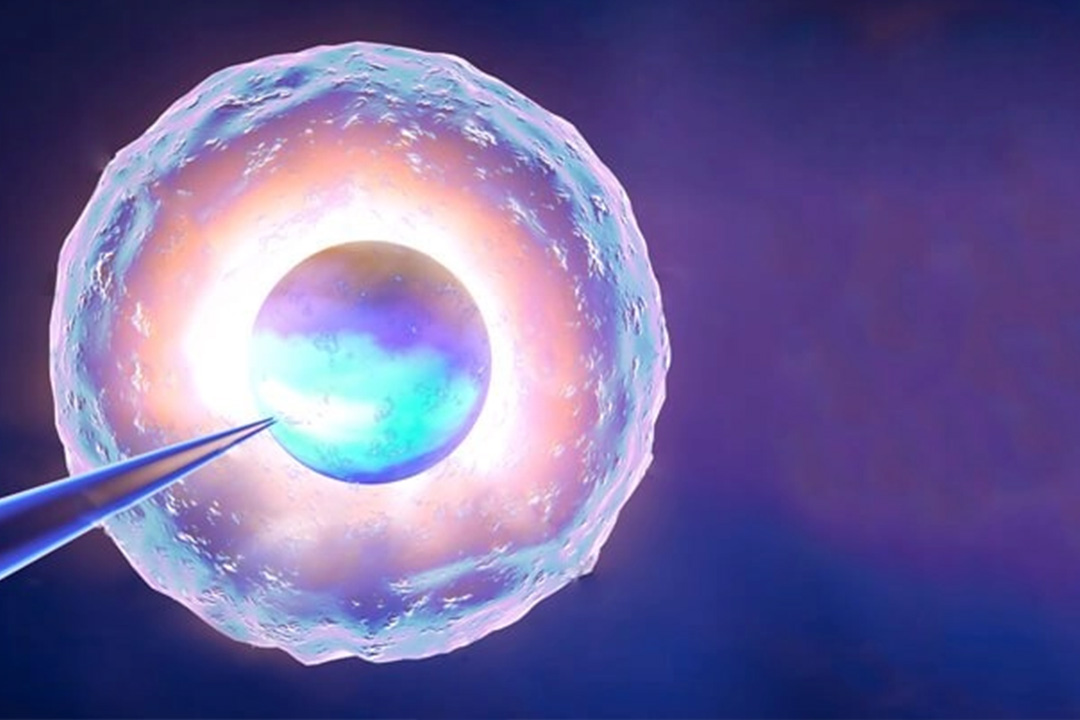
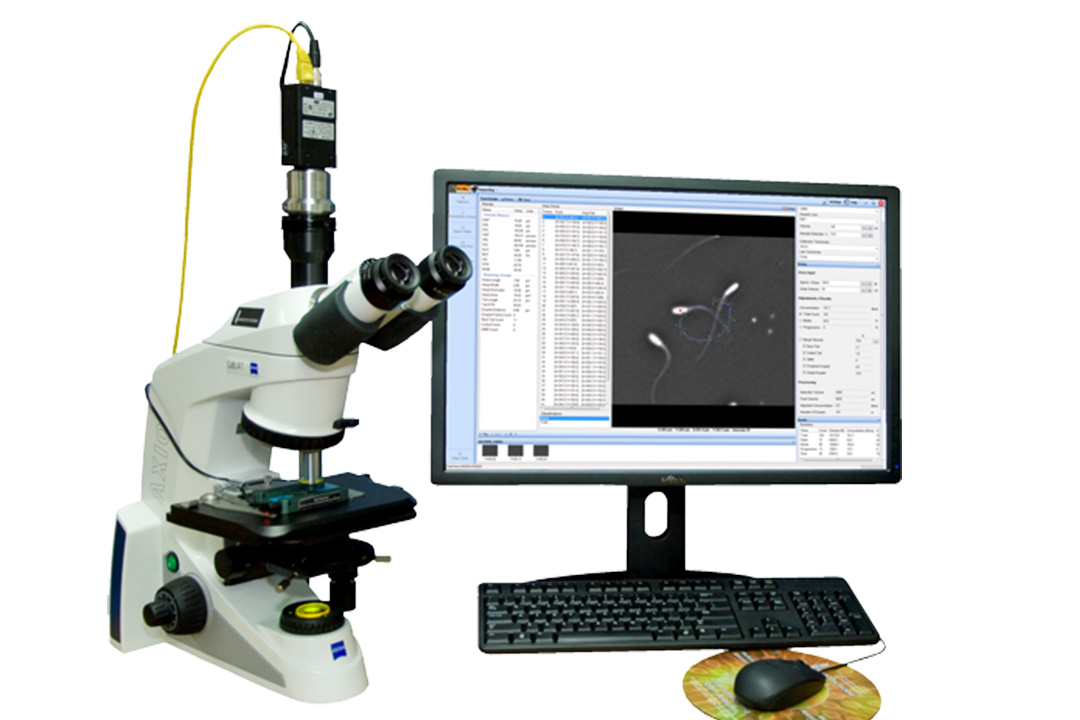
Intracytoplasmic sperm injection, as referred to commonly in shortened form as ICSI, is a derivative of IVF focusing more on addressing male factors that can lead to infertility.
In a standard IVF setting, 100,000 sperm are injected directly into the egg, while praying that at least one will properly fertilize it. However, in ICSI, a single sperm is injected directly into the egg. It is quite precise and very useful when there has been a concern over low count or poor motility of sperm.
ICSI with TESA/Micro TESE
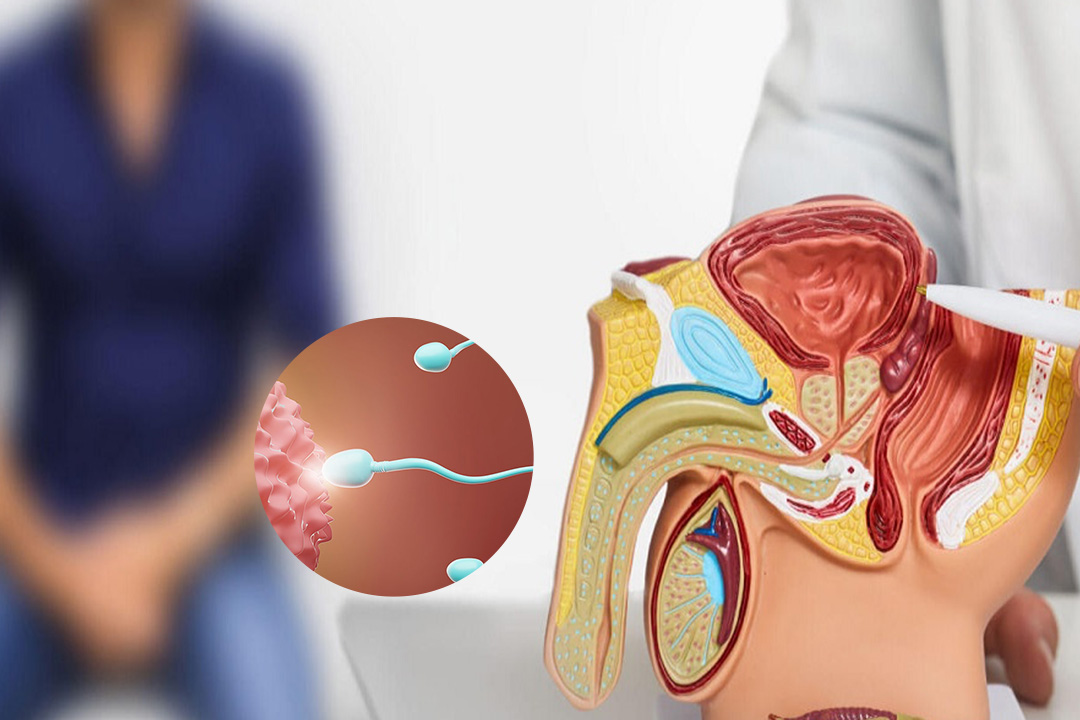
A breakthrough option, in such cases of azoospermia, where no sperm is found in the ejaculate. It is the ICSI along with Testicular Sperm Aspiration (TESA) or Micro Testicular Sperm Extraction (Micro TESE). They involve the extraction of sperm directly from the testes. The sperm can then be used to inject each egg individually in an ICSI procedure.
This procedure enables men who otherwise would not be able to contribute their genetics to have biological children. It requires rather specialized surgical procedures and expert laboratory handling but has opened the door to parenthood for many couples facing severe male infertility.
IVF with Donor Sperm
In conditions where male factors are a big hindrance for conception, use of donor sperms in the IVF treatment can be highly effective. Here, the chosen donor's sperm is used that is then fused with the egg of the female after undergoing normal IVF. This method has been very beneficial for couples wherein the male factor has a significantly low count of sperms or poor quality.
The utilization of donor sperm not only improves the chances of successful fertilization but also allows couples to successfully experience the pleasures of parenthood even when male factor infertility is the case. This is a very common option for couples and individuals, including single women and same-sex partners, who wish to build their families.
IVF with Surrogacy
IVF with surrogacy involves a third party, the surrogate mother, who carries the embryo for the intended parents. This is especially helpful for women who cannot carry a pregnancy due to medical reasons such as uterine abnormalities, severe health risks, or other contraindications to pregnancy.
The process starts with IVF, where eggs and sperm are combined to create embryos, which are then transferred into the surrogate's uterus.
Surrogacy is an alternative method for those who would otherwise not experience and enjoy pregnancy and birth. It proves to be of great value in overcoming severe reproductive failures but at the same time, guarantees that in cases where gametes are donated, the intended parents still have a genetic link with the child.
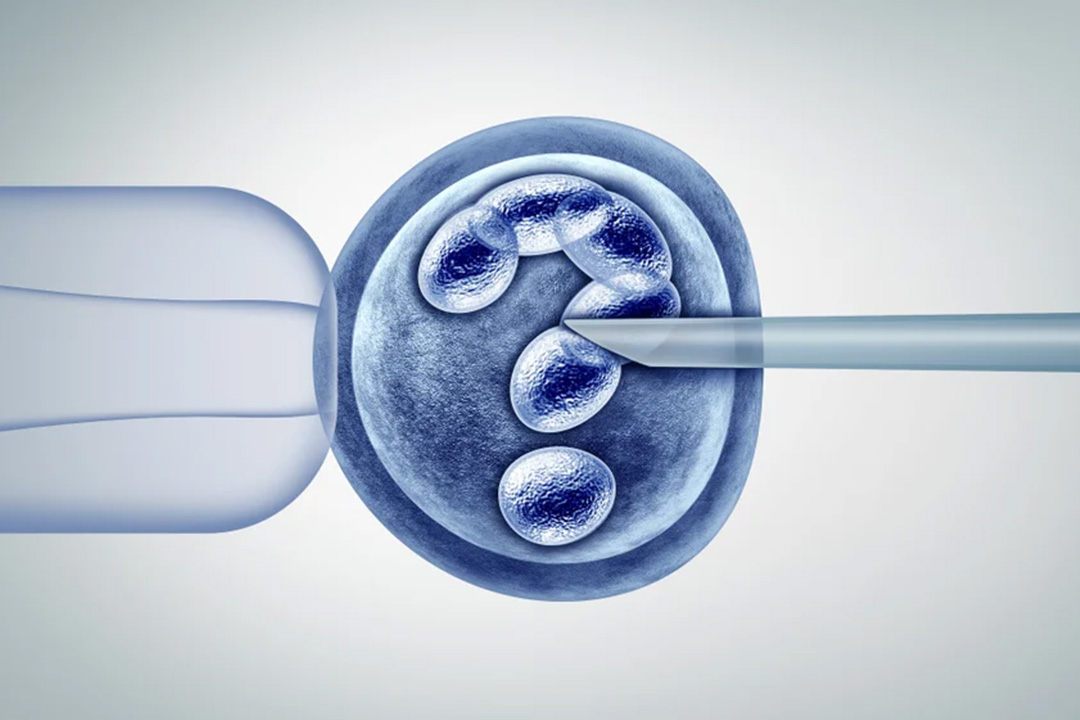
Preimplantation Genetic Testing (PGT)
Preimplantation Genetic Testing (PGT) is an advanced technique used in conjunction with IVF to screen embryos for genetic abnormalities before implantation. This procedure is recommended for couples with a history of genetic disorders, recurrent miscarriages, or previous IVF failures.
By identifying embryos with chromosomal or genetic issues early on, PGT helps in selecting the healthiest embryo for transfer, thereby increasing the chances of a successful pregnancy and reducing the risk of miscarriage.
This testing is an important tool for couples concerned about hereditary conditions. It provides peace of mind and a higher probability of having a healthy baby by ensuring that only genetically viable embryos are chosen for implantation.
Additional IVF-Related Procedures
Beyond the primary types of IVF, several additional procedures have emerged to cater to specific fertility challenges and patient preferences:
Needle-Free IVF
Needle-free IVF is a new technique developed in the goal to diminish the pain and stress generated by the traditional injection-based treatments.
Through the use of alternative routes for medication, this procedure is aimed at making IVF more friendly and less invasive without giving up the effectiveness of the treatment as a whole.
Ovarian Rejuvenation Therapy
Ovarian rejuvenation therapy aims to restore normal ovarian function to women with depleted ovarian reserve and premature ovarian failure. The underlying techniques used could stimulate the ovaries to gain quality and increased numbers of oocytes, so it would naturally enhance the overall success rates associated with subsequent in vitro fertilizations.
In vitro maturation
In vitro maturation (IVM) is a technique where immature eggs are collected from the ovaries and then matured in a setting in a specialized laboratory.
This technology is much helpful in cases where women have ovarian hyperstimulation syndrome risk or just for those who wanted a milder stimulation protocol. IVM is an alternative pathway leading to fertilization without needing long ovarian stimulation protocols.
Egg Freezing
Egg freezing, also referred to as oocyte cryopreservation, is a method that enables women to freeze their eggs for future use. The process involves retrieving and freezing eggs at a younger age, which can then be thawed and fertilized when the woman is ready to conceive.
Egg freezing is particularly useful for women who want to delay childbearing due to personal or medical reasons, ensuring that they have high-quality eggs available when needed.
The Benefits of Different IVF Approaches
Each IVF method offers unique advantages, making it possible for a wide range of patients to find a treatment plan that suits their needs. Here are some of the key benefits:
- Women with blocked or damaged Fallopian tubes can achieve pregnancy by bypassing the need for functional tubes altogether.
- For Women Older than 35, or with the Reduced Ovarian Reserve It can help patients to achieve and maximize the highest chance of obtaining conception, at a time especially when other mechanisms have failed for them.
- One in six couples suffer from undiagnosed infertility, despite extensive testing. IVF provides a means for these couples to conceive, under the expert care of fertility specialists.
- Women with conditions such as PCOS or endometriosis that can cause problems with ovulation and uterine receptivity have been treated successfully using custom IVF programs.
- For women who are suffering from early ovarian failure or reaching menopause, donor egg IVF can be a better option with a greater success rate and a chance at biological parenthood.
Conclusion
IVF has transformed the treatment of infertility, from being the 'test-tube baby' in early days to its diverse spectrum tailored to meet an individual's specific needs. Be it conventional IVF, or natural cycle protocols, minimal stimulation treatments, ICSI, genetic testing, among others, have provided a huge range of solutions to deal with various reproductive difficulties.
Whether you are opting for a traditional path or looking into more conservative, less invasive approaches such as natural or minimal stimulation IVF, the goal is the same: to provide every family with the opportunity to enjoy the gift of parenthood. With continuous research and technological advancements, the world of IVF is constantly evolving, making it one of the most promising areas in modern medicine.
About Us
AKsigen IVF is a premier center for advanced fertility treatments, with renowned fertility experts on our team. Specializing in IVF, ICSI, egg freezing, and other cutting-edge reproductive technologies, AKsigen IVF is committed to helping couples achieve their dream of parenthood. With personalized care and a patient-first approach, AKsigen IVF provides comprehensive fertility solutions under one roof.