TESA IVF: A Step-by-Step Guide to Testicular Sperm Aspiration in Assisted Reproductive Technology
Embryo Transfer in IVF
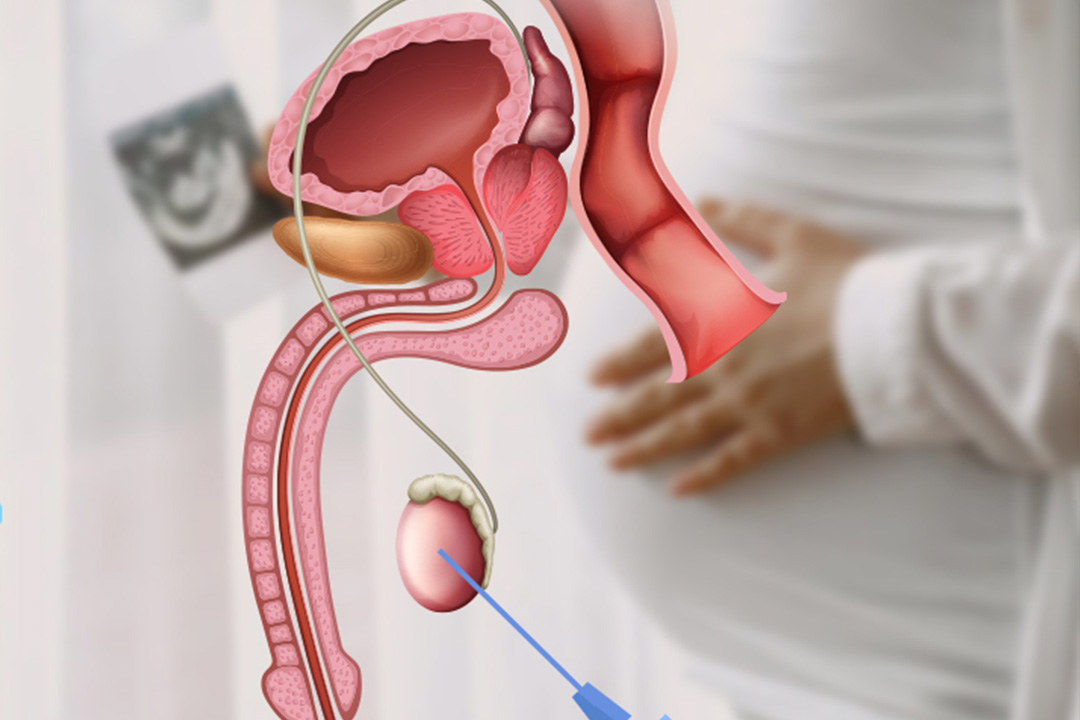
Couples feel the challenges of not being able to conceive, the search for appropriate treatment can be emotional and overwhelming. One of the new advancements in assisted reproductive technologies is TESA IVF. Testicular Sperm Aspiration (TESA) is a minimally invasive technique wherein sperm is retrieved from testicular tissue.
This guide provides an in-depth look at TESA, detailing its procedure, benefits, candidate profiles, and cost considerations, all essential information for couples considering this treatment.
Understanding Male Infertility
Male infertility is diagnosed when the couple fails to conceive despite one year of regular, unprotected sexual intercourse. Several factors lead to infertility in men: hormonal imbalances, genetic conditions, structural blockage, or lifestyle-related issues. For instance, a few men suffer from azoospermia, the absence of any sperm in the ejaculate. It can be primarily categorized into two divisions:
- Non-Obstructive Azoospermia: In this category, the testes do not produce enough sperms.
- Obstructive Azoospermia: Here, sperms are produced by the testes, but blockage prevents it from entering into the ejaculate.
In case of obstructive azoospermia, procedures like TESA provide promising avenues for collecting sperms directly from the tissue of the testis, without passing through any obstruction. For such couples wishing to improve fertility with advanced Assisted Reproductive Techniques, TESA represents an important route.
What Is TESA?
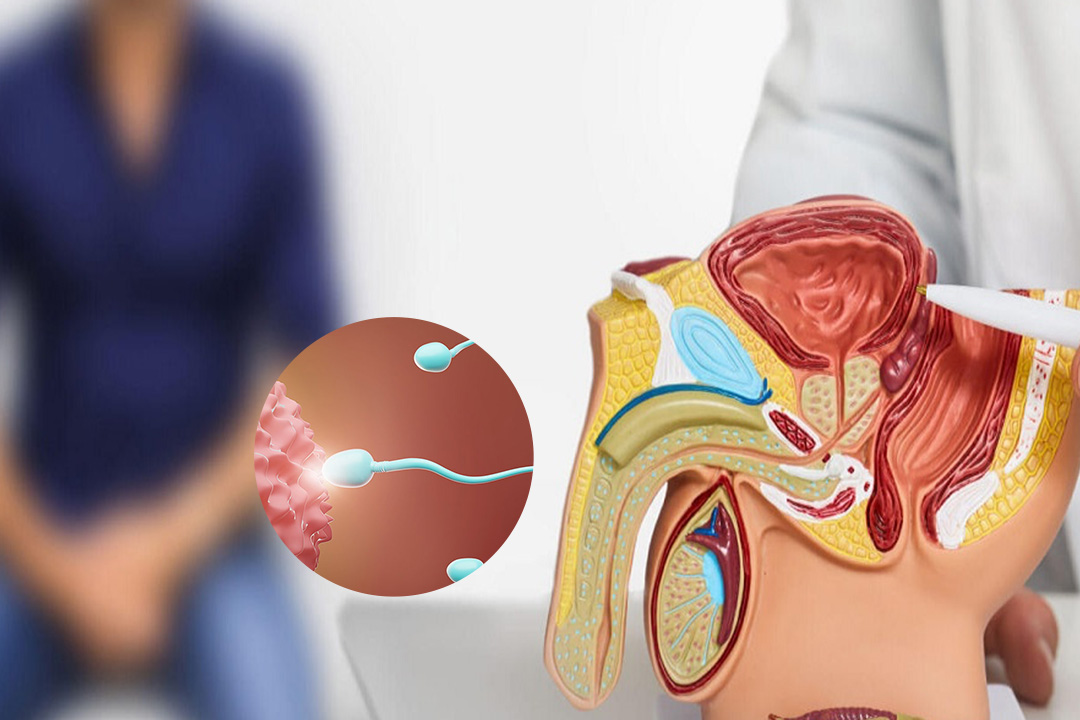
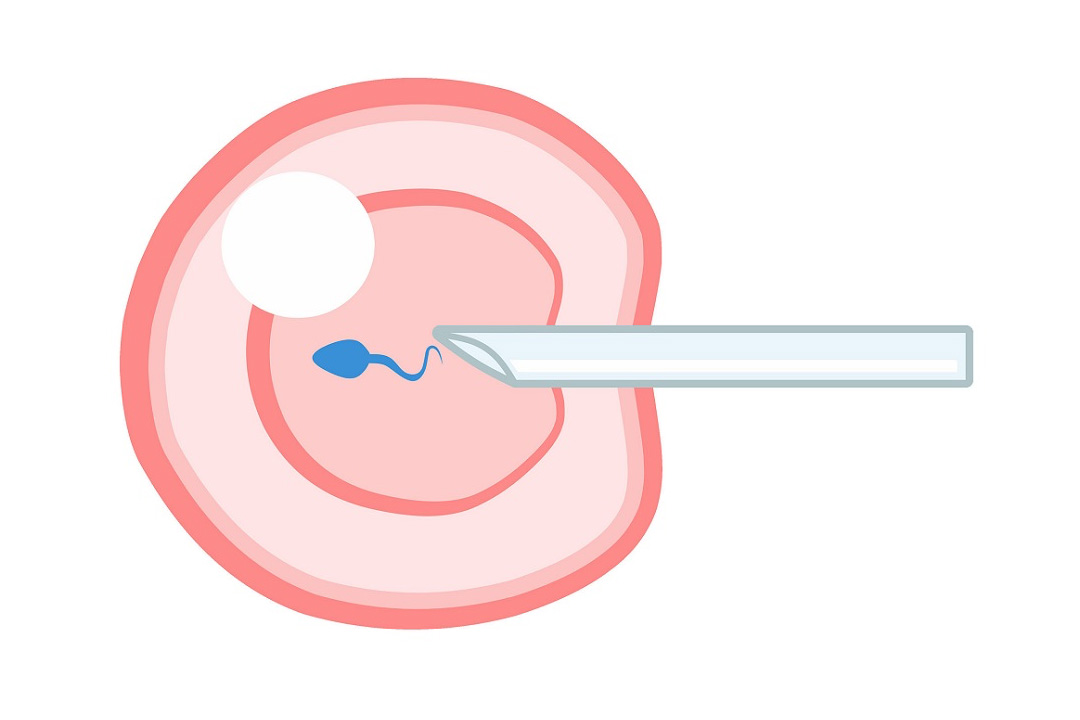
TESA stands for Testicular Sperm Aspiration. It is a surgical process where sperm-rich fluid is aspirated from the testicle through a fine needle. The entire process is generally carried out with local anesthesia to ensure that there is minimal pain experienced by the patient during this process.
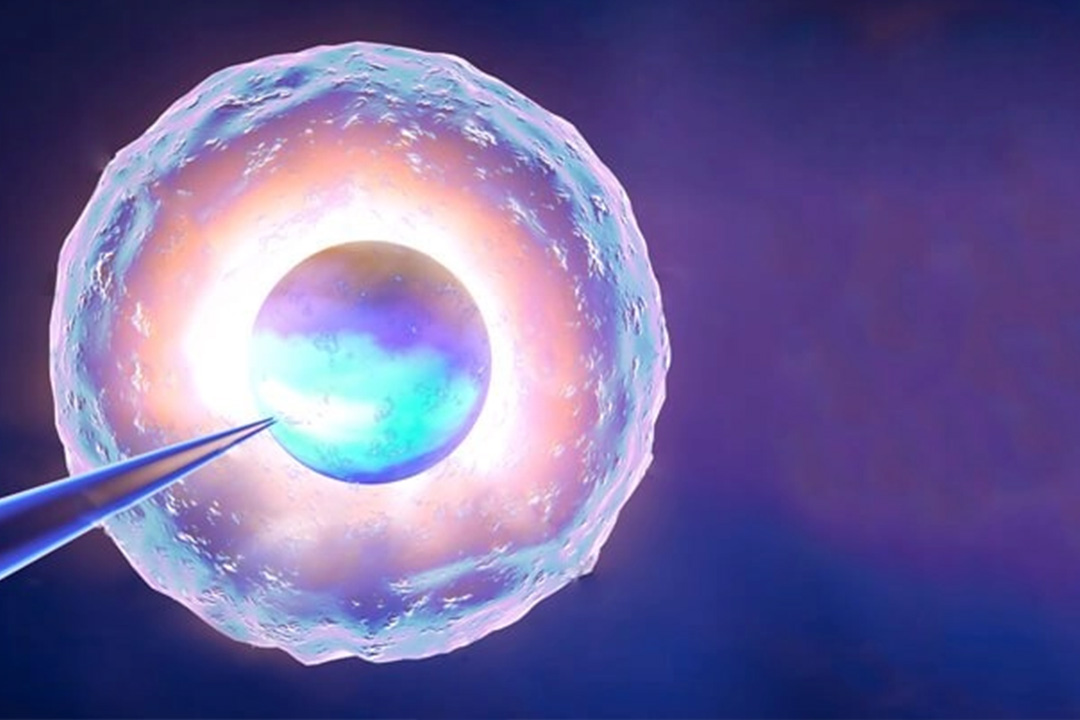
When the fluid has been aspirated, embryologists analyze it using a microscope in order to select viable sperm which can be further used in ICSI, one of the common fertility treatments.
This procedure is especially beneficial when other methods of sperm retrieval, like conventional semen collection or PESA (Percutaneous Epididymal Sperm Aspiration), have failed or are not suitable due to the nature of the male infertility.
Pre-Procedure Preparations
Before undergoing TESA, patients must go through several preparatory steps to ensure the procedure is both safe and effective. These steps include:
1. Medical Consultation
A comprehensive consultation with a fertility specialist forms the initial stage. At this point, the specialist consults and examines the medical history of the patient, discusses the issues associated with infertility the couple faces, and identifies any problems present for determining the causes of the issue that necessitates TESA to be used for treatment.
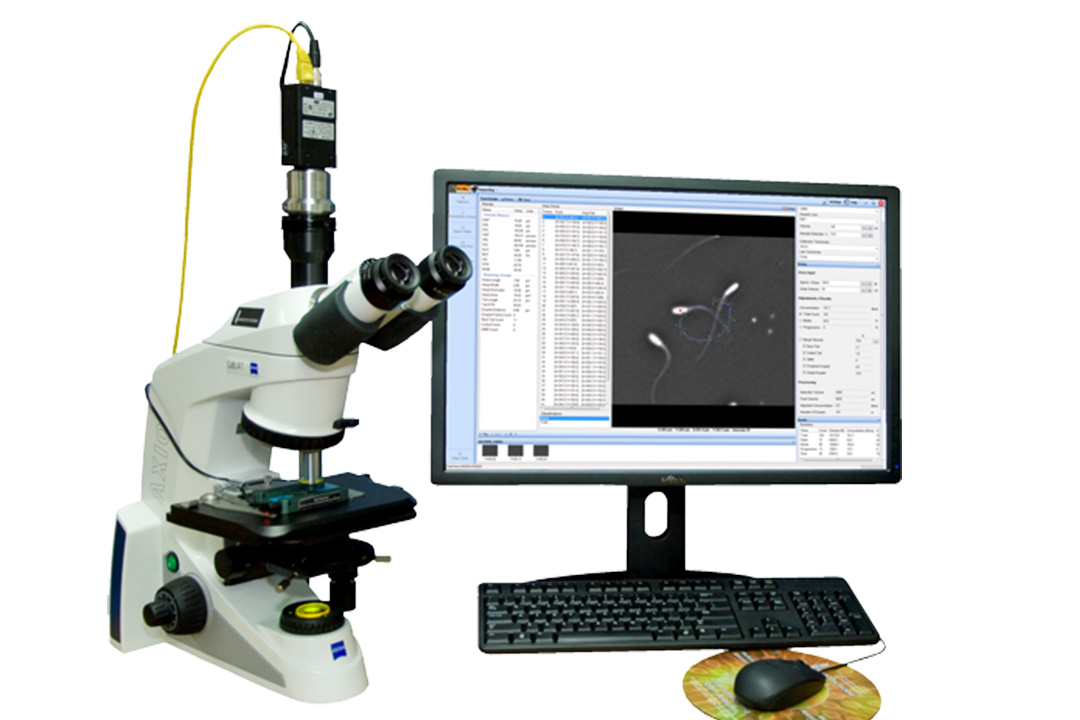
2. Semen Analysis
A detailed semen analysis is generally performed to check for sperm count, motility, and morphology. The test results give information regarding the degree of the male factor infertility and also indicate if the sperm need to be extracted directly.
3. Hormonal and Genetic Testing
In some cases, blood tests are conducted to check hormone levels or to identify any genetic conditions that might be contributing to the infertility. These tests ensure that any underlying issues are understood and appropriately managed.
4. Counseling
Both partners usually need counseling to grasp the TESA procedure, risk, benefits, and outcome. This is necessary for managing expectation and ensuring the couple is satisfied with the whole process of the decision-making.
5. Drugs
The doctor may prescribe medicines that can either increase sperm or improve the sperm quality. Some of these preparations may increase the chances of taking viable sperms during the process of TESA.
The Process of TESA: Step to Step
The TESA procedure is performed with the intention of being minimally invasive and time-saving. The key steps of this procedure are as follows:
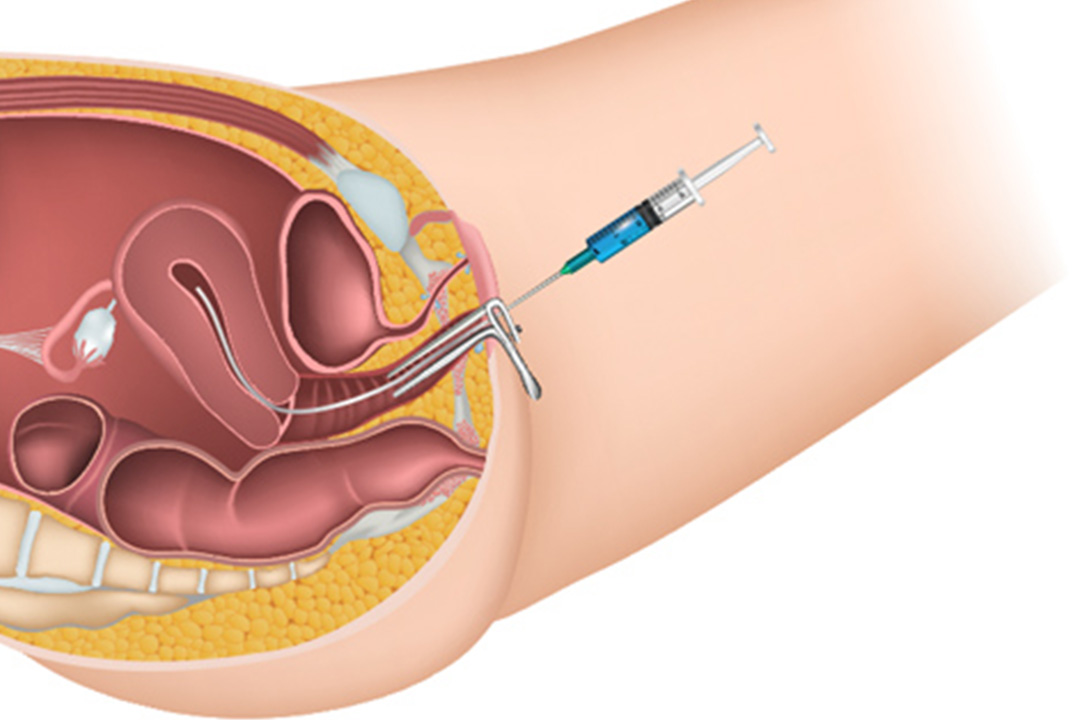
1. Administration of Local Anesthesia
For comfort of the patient, local anesthesia is given in the testicular area. This numbs the area, thereby making it less painful for the procedure.
2. Needle Aspiration
A fine needle is carefully inserted into the testicle. The specialist then applies gentle suction to extract a small amount of testicular tissue or fluid, which contains the sperm.
3. Sperm Isolation and Extraction
Once the aspirated fluid is collected, it is immediately transported to the laboratory. Here, embryologists examine the sample under a microscope and carefully isolate viable sperm. This step is critical, as even in cases of severe male infertility, small quantities of healthy sperm may be present.
4. Sperm Preservation
After extraction, the obtained sperm can be utilised immediately through assisted reproductive techniques like ICSI. Alternatively, the sperm may be cryopreserved and used later, allowing for flexibility in planning subsequent fertility treatments.
Advantages of TESA in Fertility Treatment
TESA gives couples facing male infertility several important benefits. The key advantages are :
1. It is an effective method of sperm retrieval.
Even if the sperms are not available in the semen because of obstructions in the epididymis and vasa or there is significant malformation in sperms, viable sperms can still be recovered directly from the testes using TESA.
2. Minimal Invasive Procedure
TESA requires a tiny puncture using a thin needle, and therefore it is minimally invasive. It limits the complications, and usually recovery is much less time-consuming as compared to surgical methods.
3. More Assisted Reproductive Options
The sperm aspirated through TESA can be employed for various assisted reproductive techniques. For instance, in an ICSI cycle, a single sperm may be injected directly into the egg. This significantly improves fertilization chances even if the quality of sperms is poor.
4. Cryopreservation Flexibility
One of the major advantages of TESA is that the extracted sperm can be frozen for future use. This is especially valuable if the couple decides to delay the next stage of treatment or if multiple cycles of fertility treatment are anticipated.
Who Should Consider TESA?
TESA is not a one-size-fits-all solution but is particularly beneficial for specific infertility scenarios. The following groups are most likely to benefit from TESA:
1. Obstructive Azoospermia
Patients who have a blockage preventing sperm from accessing the ejaculate, yet whose testes are producing normal amounts of sperm, are best treated with TESA. Many of these patients have Congenital Bilateral Absence of the Vas Deferens (CBAVD), a very suitable candidate for TESA.
2. Failed Sperm Retrieval Patients
For men who have undergone other sperm retrieval methods, like PESA, without success, TESA offers an alternative route to obtain viable sperm.
3. Severe Cases of Oligo-Astheno-Teratozoospermia (OATS)
Patients with extremely low sperm counts, poor motility, and abnormal sperm morphology may benefit from TESA. Studies have indicated that testicular sperm retrieved via TESA may exhibit better integrity and quality compared to sperm found in the ejaculate.
4. Cases of Cryptozoospermia
Men with cryptozoospermia—where sperm are rarely observed in the ejaculate—might have better outcomes with TESA since it can extract sperm directly from the source, potentially bypassing damage incurred during transit through the reproductive tract.
Potential Side Effects and Safety Considerations
TESA is known for its safety and minimal invasiveness. However, like all medical procedures, it does come with a few risks and potential side effects:
- Minor Discomfort
- Swelling or Bruising
- Rarer Anesthesia-Related Problems
It must be remembered that long-term complications from TESA are extremely rare. Most patients recover rapidly and return to normal activities within a few days.
Cost Factors Involved in TESA
Among many other aspects for couples, financial investment for treatments is very significant. TESA cost will be different in a variety of different factors like place, experience level of the team, and processing and freezing sperm in laboratory besides the initial TESA. Role of TESA in Advanced IVF Techniques.
In many cases, TESA is performed in conjunction with Intracytoplasmic Sperm Injection (ICSI), an advanced IVF technique where a single sperm is injected directly into an egg. This combination is particularly effective when traditional methods of fertilization are unlikely to succeed due to issues with sperm quality or quantity. By using sperm retrieved directly from the testes, embryologists have a higher chance of achieving successful fertilization, which can lead to improved embryo quality and increased pregnancy rates.
The integration of TESA with IVF treatments demonstrates the rapid advancements in reproductive medicine. It not only offers hope to couples dealing with male infertility but also expands the range of available options to tailor treatments according to each patient’s unique needs.
Conclusion
TESA IVF is a powerful tool in the realm of assisted reproductive technology. For couples facing challenges due to male infertility, especially in cases of obstructive azoospermia, severe OATS, or cryptozoospermia.
TESA offers a minimally invasive, effective method for retrieving viable sperm. Its integration with advanced techniques such as ICSI further enhances the prospects of achieving a successful pregnancy.
The decision to undergo TESA should be made after thorough consultations and diagnostic evaluations. With modern advancements, the procedure is safe, with minimal discomfort and a swift recovery period.
Furthermore, the ability to cryopreserve sperm provides additional flexibility in planning future treatment cycles, ensuring that couples are supported throughout their journey toward parenthood.
About Us
AKsigen IVF is a premier center for advanced fertility treatments, with renowned fertility experts on our team. Specializing in IVF, ICSI, egg freezing, and other cutting-edge reproductive technologies, AKsigen IVF is committed to helping couples achieve their dream of parenthood. With personalized care and a patient-first approach, AKsigen IVF provides comprehensive fertility solutions under one roof.